Introduction
Sarcomas of the head and neck region are found to be present in only 1% of all head and neck malignancies.1 Rhabdomyosarcoma (RMS) predominantly occurs in children (60%) while it is rarely found in the adults (2%–5%).2, 3 The common sites of occurrence are the head and neck region (35%), genitourinary tract (23%), retroperitoneum and the extremities (17%).4 In the oral cavity, it mostly involves the tongue followed by soft palate, hard palate and the buccal mucosa, may also involve the gingiva in very rare cases.2, 4 RMS of oral cavity are rare accounting for about 10% of all cases.
The main sites of origin for RMSs of the head and neck are: orbit, middle ear, nasal cavity, paranasal sinuses, nasopharynx and infratemporal fossa. According to the site of origin, the RMS of the head and neck can be divided in three subtypes: Para meningeal, non parameningeal and orbit. Para meningeal sites are those adjacent to meninges as nasal cavity, paranasal sinuses, nasopharynx, middle ear/mastoid, parapharyngeal space, infratemporal fossa and pterygopalatine fossa. Oral cavity, oropharynx, face, cheek, parotid region and soft tissue of the neck are considered nonparameningeal sites.5
Histologically, the RMSs can be divided in embryonal, alveolar and pleomorphic. The embryonal type presents the subtypes such as classic, spindle cell and botryoid. The embryonal RMS is composed of several cell types and the mesenchymal cells tend to differentiate into cross-striated muscle cells. It is generally a moderately cellular tumor with loose myxoid stroma. The cell nuclei of embryonal RMS are smaller than those of an alveolar RMS and the nucleoli are difficult to visualize. The immunohistochemical positivity for vimentin, muscle specific actin, desmin and mioglobin has been used to distinguish RMS of other soft tissue sarcomas with similar histopathological patterns.6
Case Report
A 22 year old male patient reported to the Department of Oral and maxillofacial Pathology with a swelling and obvious asymmetry of the right side of the face for three weeks after extraction of maxillary teeth. The patient had a history of khaini chewing with gutkha. These are forms of chewing tobacco available widely and easily. The patient had undergone an FNAC from the lesion and a report of Squamous cell carcinoma was given with a note for urgent biopsy to confirm the lesion.
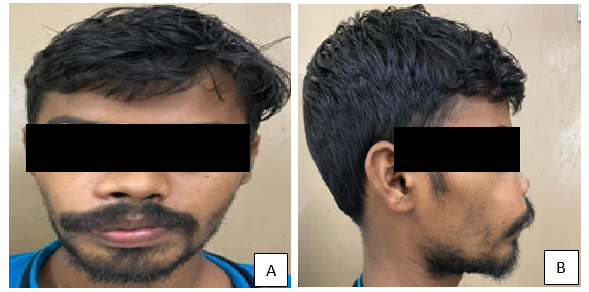
On examination, there was obvious extra oral asymmetry of the face (Figure 1A). The right nasolabial fold was obliterated (Figure 1B). Intra orally, there was a fleshy mass of the right upper alveolar ridge in the lateral incisor and canine region. Both the teeth had exfoliated. The lesion extended towards the palate as well as Buccal vestibule and showed rapid growth with a size of more than 3cm by 4cm. There was no ulcerated lesion or obvious granular surface or keratinisation (Figure 2).
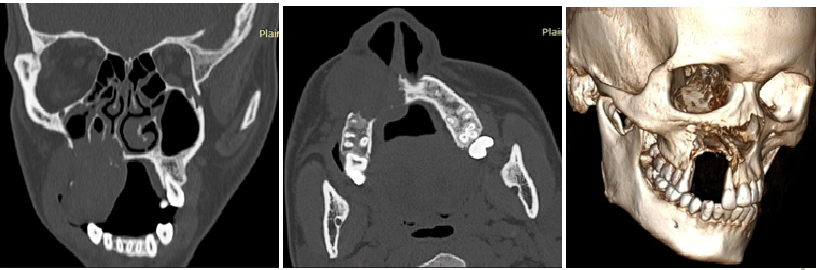
CT Scan of the face showed an expanding, well-defined, destructive lytic lesion (3.6x3.5x4.2cm) involving alveolar and palatine process of right maxilla and anterior & medial walls of right maxillary sinus, right gingivo-buccal complex, part of right buccinator muscle and the right nasolabial fold with bone destruction. In addition, bony nasal septum was slightly deviated towards the right. The radiological findings were consistent with a neoplastic etiology (Figure 3).
After routine blood examinations, Incisional biopsy was done from the lesion under local anaesthesia. A mucosa covered irregular piece of tissue was sent for histopathology. There was no healing of the biopsy wound (Figure 4).
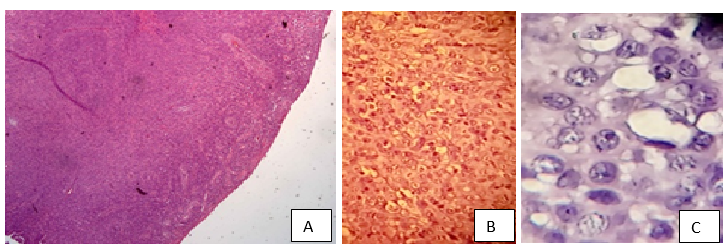
Section stained with H&E revealed the presence of sheets of polygonal to plump spindled cells having high nuclear cytoplasmic ratio, vesicular nuclei with opened up chromatin and amphophilic cytoplasm. A fair number of mitotic figures are present. No necrosis was seen. Gland formation or Squamous differentiation has not been identified. Overlying Squamous epithelium was ulcerated. A diagnosis of poorly differentiated malignant neoplasm was given (Figure 5A,B,C). Immunohistochemistry (IHC) was recommended for exact categorisation.
One paraffin block and one stained slide (H&E) were sent for IHC to higher centre. They found very high mitotic rate (18/10 hpf). A large panel of markers was done. Tumor cells express Vimentin, Desmin and Myo D1 (Figure 6). Ki-67 index was 50%. The tumor cells are immunnonegative for Pan CK, S-100 protien, HMB 45, CD34, Synaptophysin, CD45, TLE1, SATB2, ERG, CD31, SMA, Myogenin, EMA, SOX10, CD 99 and NTRK. The impression was that based on IHC and H/P and lack of any obvious pattern, the lesion was given a diagnosis of Rhabdomyosarcoma (NOS). As no definitive pattern of the cells was found, the final diagnosis was given as Pleomorphic Rhabdomyosarcoma.
Discussion
Oral Squamous cell carcinoma is the most common cancer in India which provides almost one third of the total burden seen worldwide.7 Among Oral cancers it is the commonest and 96% of all oral malignancies are Squamous cell carcinomas. Tobacco consumption both in the form of smoking and smokeless are the major causes and risks associated with oral Squamous cell carcinoma. Bidi smoking and alcohol consumption lead to higher risk of development of oral cancer.8 In the present case, the patient had a history of smokeless tobacco use. A FNAC was advised which revealed some aggressive cells and based on this presumption, a preliminary diagnosis of Oral Squamous cell carcinoma was done. This was completely off the mark. Many important issues come into play with this finding. Firstly, it is wrong to assume that all oral cancers are Squamous cell carcinoma. Secondly, comes the importance of IHC in the advanced diagnostic techniques which is important for the diagnosis in these cases. Thirdly, correct diagnosis is very important for the final treatment planning of the patient.
In general, the commonest age for development of Oral cancer in India was 5th decade of life.9 Hence; it is not very common for Oral Squamous cell carcinoma to develop at the age of 22. Moreover the lesion was smooth surfaced and did not show any ulceration or keratinization prior to biopsy.
Although the management of OSCC and RMS is almost alike, the ability of metastasis is salient compared to OSCC. Therefore, the definitive diagnosis should be careful due to its characteristic.10
For the definitive histological interpretation of Pleomorphic RMS, giant cell or multinucleated myoblasts, strap or tadpole cells and pleomorphic individual tumor cells with or without cross-striations with congested eosinophilic cytoplasm, are some of the common required features. However, in most circumstances, RMS tends to display wide features of histological presentation with poor differentiation, often making diagnosis and interpretation difficult.11
Majority of oral RMSs are of embryonal type, composed by small, round‑to‑oval tumor cells with finely granular eosinophilic cytoplasm. Besides, the well differentiation shows elongated, strap‑shaped or tadpole‑shaped rhabdomyoblasts. Giant cells with enlarged or multiple nuclei can also be found. Mitotic figures are often seen and may be abnormal. The stroma of tumor is minimal and consists of moderately loose to dense fibrous tissue. Alveolar RMS is typically consisted of small round densely packed cells, organized around spaces resembling pulmonary alveoli. A solid variant form of alveolar RMS consists of small round densely packed cells without the characteristic alveolar spaces. Pleomorphic RMS is rarely diagnosed and is characterized by pattern less of large amount of anaplastic cells, roundcells and spindle cell.12
RMS in adults have poor prognosis as compared to childhood RMS. Adult RMS should therefore be treated aggressively with multidisciplinary approach comprising of surgery, radiation and chemotherapy to achieve cure and prolonged survival.13
Conclusion
In this case, histopathological and immunohistochemical examination is mandatory because of clinically resembling OSCC lesions. As Squamous cell carcinoma is the most common oral malignancy, there is a tendency for diagnosing lesions with a bias. Also it was noted that FNAC is inadequate in diagnosing these type of lesions. The marked pleomorphic nuclei and IHC results were critical for differentiating RMS from others. The management needs multidisciplinary case approach in collaboration with colleagues.