Introduction
Oral pyogenic granuloma is a prevalent gingival tumour with a 75% predilection in gingiva. The primary etiologic feature is found to be dental calculus and foreign materials in the gingival sulcus. The maxilla has slightly more lesions than the mandible. Other prevalent locations include the lips, tongue and buccal mucosa.1, 2 The size ranges from a few millimetres to several centimetres and it typically grows slowly, asymptomatically and painlessly, although it can also grow quickly.3
Pyogenic granuloma, formally known as granuloma pyogenicum is a benign and soft vascular proliferation typically observed as a solitary growth on the skin or within the oral cavity. It has been designated by various alternative names, including granuloma pediculatum benignum, pregnancy tumour, vascular epulis, Crocker and Hartzell’s disease. The current nomenclature, "pyogenic granuloma," was officially coined by Crocker in 1903, while Hartzell introduced the term "granuloma pyogenicum" in 1904.4
Some investigators categorize pyogenic granuloma as a "reactive" or "reparative" tumour process. As proposed by Regezi et al., pyogenic granuloma is described as an exuberant growth of connective tissue in response to a known stimulus or injury, such as calculus or foreign material within the gingival crevice.5 Numerous "etiologic factors," including trauma, injury to a primary tooth, chronic irritation, hormonal influences, medication effects, gingival inflammation, preexisting vascular lesions, chronic irritation due to the exfoliation of primary teeth, eruption of permanent teeth, defective fillings in the proximity of the tumour, food impaction, periodontitis, toothbrush trauma and others have been identified as potential causative factors when patients present with these clinical findings.1 In this article, we have presented a case report of an exorbitant pyogenic granuloma of the gingiva in a 62‑year‑old female patient who reported with a vivid vascular tumour like growth in upper anterior region which was managed by surgical excision followed by histopathological investigation.
Case Report
A 62-year-old female patient reported to the out-patient Department of Periodontology with a chief complaint of painful swollen gums for the past 1 month. Patient gave history of pain which was of gradual onset, moderate intensity, continuous in nature, aggravated by mastication and relieved by rest. She gave a medical history of diabetes mellitus and under regular medication for the past 2 years. Patient gave history of tooth extraction and replacement with removable denture before 5 years in lower anterior region. Her family history was non-contributory. Hormonal history revealed that the patient had attained menopause before 7 years. Extra oral examination revealed an apparently symmetrical face with potentially competent lips. Right and left sub mandibular lymph nodes were palpable and tender which were soft in consistency.
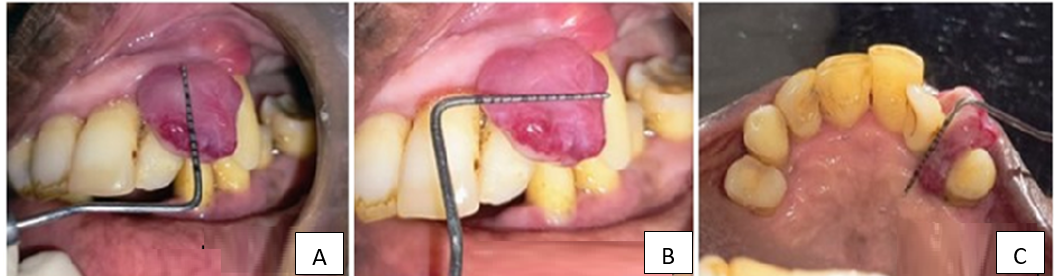
Intra oral examination revealed a single pedunculated swelling of size 1.5 x 1.5 cm on the labial aspect of gingiva in relation to 22,23 extending into the palate between 22, 23 (Figure 1A,B,C). It was bright red in colour with smooth texture and profusely bled on slight provocation. On palpation, the swelling was soft in consistency with tenderness, non-pulsatile and blanches on pressure. Oral hygiene status of the patient was poor. Gingival examination showed generalized erythematous marginal gingiva, loss of scalloping with blunt interdental papilla and rolled marginal gingiva. Bleeding on probing was generalized. Hard tissue examination revealed decayed tooth in relation to 47, missing teeth in relation to 15,16,17,25,26,27,28,31,41,42, Grade III mobility in relation to 22,23,18, Grade I mobility in relation to 11,13,33,34,43,46,47,48. IOPA of 22,23 revealed radiographic bone loss extending till apical third of the tooth with widening of periodontal ligament space and loss of lamina dura. OPG revealed generalized horizontal bone loss with missing teeth. (Figure 2A,B) with the above mentioned history and clinical presentation, the lesion was provisionally diagnosed as generalized chronic periodontitis as lobular capillary hemangioma in relation to 22,23 - ?. Differential diagnosis was given as pyogenic granuloma, Peripheral ossifying fibroma.
Treatment done
Informed consent and medical opinion were obtained. Phase I therapy consisting of scaling and root planing was done following which antibiotics were prescribed. Patient was subjected to routine hemogram and diabetic status was assessed and no abnormalities were detected. Patient was then posted for surgical excision.
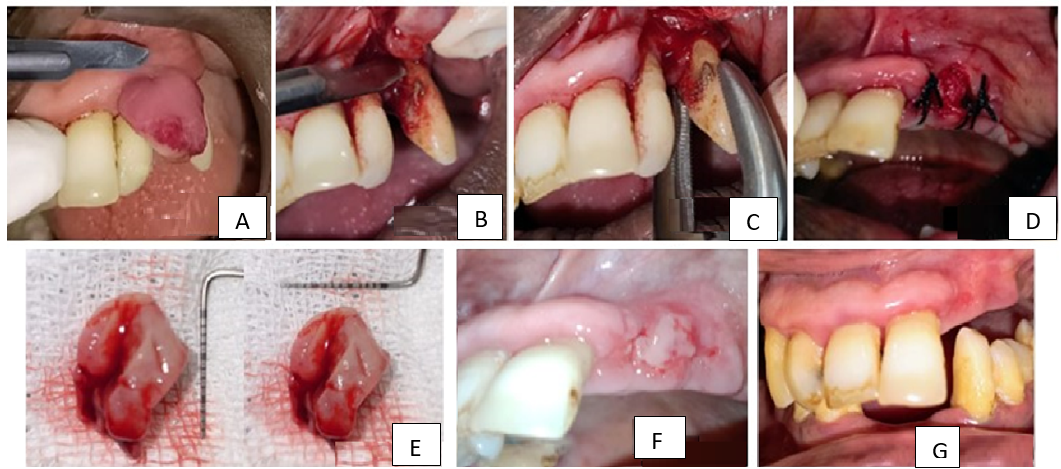
Surgical phase
Buccal and palatal infiltration anesthesia was given using lignocaine hydrochloride with 1:80000 adrenaline. Under LA bleeding points were marked on the buccal and palatal aspect of the gingiva. Incision was made using no. 15 blade apical to the bleeding points marked in relation to 22,23 (Figure 3A), full thickness dissection was done and the lesion was excised along with 1mm of normal tissue and sent to biopsy (Figure 3B, E). 22,23 were extracted and the area was thoroughly debrided for removal of any remnant tissue (Figure 3C). Area was irrigated with copious betadine- saline and simple interrupted sutures were placed using 3-0 silk (Figure 3D). Patient was instructed to refrain from brushing in that area for 1 week. Cap. Amoxicillin 500 mg 8th hourly and Tab. Aceclofenac and paracetamol (100mg + 325mg) was given 12th hourly to the patient for a period of 5 days. 0.2% Chlorhexidine mouth wash was given and instructed to use twice a day, after a day of the surgery. Patient was recalled after 1 week for suture removal. At 7th day, suture removal was performed and oral hygiene was reinforced to the patient and the patient was motivated for removal of hopeless teeth and prosthetic rehabilitation (Figure 3F). 1 month follow showed complete uneventful healing of the site (Figure 3G).
Histopathological examination
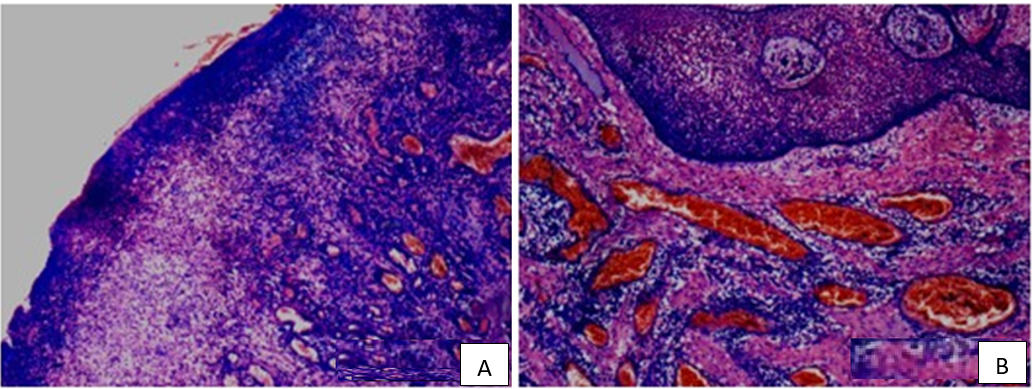
Histopathological examination revealed keratinized stratified squamous epithelium showing pseudo-epitheliomatous proliferations with connective tissue entrapments in the epithelium. Connective tissue stroma showed varying sized and shaped capillaries and proliferating endothelial cells. Numerous chronic inflammatory cells were seen suggestive of pyogenic granuloma (Figure 4A,B).
Figure 2
A): OPG reveals generalized horizontal bone loss, B): IOPA 22, 23 reveals alveolar bone loss extending till apical third i.r.t to 22,23

Figure 3
A): Incision made using No. 15 sterile surgical blade, B): Full thickness mucoperiosteal reflection and excision of the lesion, C): Extraction of 22,23, D): Flap approximation and suturing using 3-0 braided black silk, E): Excised lesion, F): Post-operative healing after 1 week after suture removal, G): Post-operative healing after 1 month
Discussion
The present case report describes about a vivid vascular growth in the maxillary anterior region. When a mass is found in the oral cavity, formulating a differential diagnosis plays the major role. However, the biopsy report confirms the diagnosis. The histopathological findings in the present case were suggestive of oral pyogenic granuloma.
The present case mimicked lobular capillary hemangioma with a clinical presentation of erythematous exophytic lesion on maxillary gingiva affecting individual in age group between 50 and 70yrs, pedunculated 1.5cm in size, painful with profuse bleeding on slight provocation.6 It is quite difficult to distinguish the two lesions based on the clinical findings since they share common clinical characteristics. However, the histopathological examination could be confirmative. The mean vessel diameter in pyogenic granuloma is 19µm where as it is 9 µm in lobular capillary hemangioma.7 The differential diagnosis in this case could be peripheral ossifying fibroma, hyperplastic gingival inflammation, peripheral giant cell granuloma (PCCG), metastatic cancer, haemangioma, angiosarcoma.1
It is now widely believed that Pyogenic granuloma is caused by an excessive locale-specific connective tissue reaction to a slight injury or any underlying irritation. Calculus, poor dental hygiene, nonspecific infection, overhanging restorations, cheek biting and other factors can all cause irritation. Because of this irritation, the underlying fibrovascular connective tissue becomes hyperplastic and granulation tissue proliferates, leading to the emergence of a pyogenic granuloma.8
According to Vilmann et al, nearly all of the pyogenic granulomas are located on the marginal gingiva, with just 15% of the tumours on the alveolar portion.9 Pyogenic granuloma (PG) is treated surgically by a thorough excision. The recurrence of PG can occur with a recurrence rate of 16% among treated lesions and hence re-excision of such lesions may be necessary.3
Al-Noaman in his study explored the clinicopathological and treatment scenario of pyogenic granuloma and concluded that the lesion shows peak incidence in fourth decade of life with a recurrence rate of 14.3% at 1 year follow-up.10 Koel et al managed recurrent pyogenic granuloma with platelet rich fibrin membrane in order to prevent osteoclastic bone resorption at surgical site, to aid in wound healing and improve patient comfort.11
Various treatment methods have been advocated in excision of pyogenic granuloma which includes use of electrocautery, soft tissue LASERs, cryosurgery etc which are equally effective as that of conventional techniques.12
Conclusion
Though the clinical presentation of the lesion may mimic various other lesions, at times a large lesion could even have a simpler diagnosis. It is important for the clinician to have sound knowledge about the differential diagnosis in order to provide adequate patient care. Scalpel excision of Pyogenic Granuloma is a safe and clinically successful procedure. To effectively treat recurrent lesions, it's important to address the underlying causes while minimizing injury to the surrounding vital structures.