- Visibility 229 Views
- Downloads 15 Downloads
- DOI 10.18231/j.ijohd.2024.009
-
CrossMark
- Citation
Non - extraction treatment of class ii division 2 malocclusion with forsus fatigue-resistant device – 2 case report
- Author Details:
-
Vaishanavi Mahajan *
-
Isha Aggarwal
-
Sanjay Mittal
-
Merry Goyal
-
Abida Parveen
Introduction
For orthodontists, Class II malocclusion is a significant and frequent challenge. This malocclusion is defined as a distal relationship between the mandible and maxilla with a variety of dental and skeletal components that may negatively impact facial function and appearance. This malocclusion was further separated into divisions 1 and 2 based on the relationship between the incisors. [1], [2], [3]
Distocclusion, increased overbite, labioversion of the maxillary lateral incisors, retroclination of the maxillary central incisors, and a more normal lip function are characteristics of class II division 2. While Division 1 malocclusion is retrognathic, the facial skeleton is not. The lack of adequate occlusal stops for the eruption of lower incisors and the deepbite that results in Class II Division 2 patients are both factors that contribute to increased overbite. These patients also exhibit more acute crown root angulation (Collum angle) as a result of a high lower lip line, which causes the crown of the tooth to deflect following eruption in relation to the root. Class II malocclusions can be corrected with removable or fixed functional appliances depending on the antero-posterior discrepancy and cooperation and growth status of the patient.
Fixed functional appliances are typically used to treat patients who have finished growing and those with Class II mandibular retrusion since they need little patient cooperation. Recently, a number of Class II correctors have been introduced that lessen or do away with the requirement for patient compliance.
Fixed appliances are a superior choice since they are less obtrusive, operate continuously, and can be used in conjunction with multibracket therapy to effect modifications in a single phase. Fixed functional appliances come in three different types: rigid, flexible, and hybrid. The combination of maximum strength and flexibility in hybrid fixed functional appliances makes them an excellent choice for treating Class II malocclusion. [4], [5], [6], [7]
Forsus Fatigue Resistant Device (FRD), one of many treatment options for Class II malocclusion caused by mandibular retrusion in growing patients, has recently become extremely popular due to its non-compliant design and effective treatment outcomes. William Vogt invented the Forsus FRD, a hybrid fixed functional appliance with a telescoping system that incorporates a super-elastic nickel-titanium coil spring and can be put together quickly at the chair. The push rod can be positioned either distal to the canine or the first premolar bracket while the spring is attached to the distal of the maxillary first molar, allowing the jaw to move forward more easily. Many studies have shown favourable results with the use of forsus during post-pubertal growth period showing its effect on restraining maxillary growth, distal movement of maxillary arch, stimulating mandibular growth and mesial movement of mandibular arch. [8], [9], [10]
Case Report
Case-1
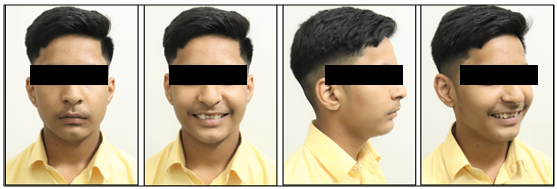
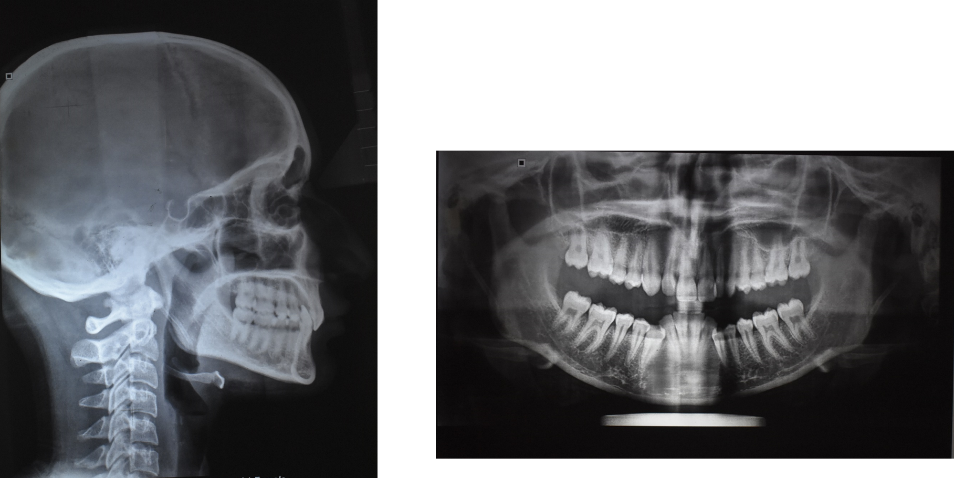
A 14 year old male patient reported to the department with chief complaint of irregularly placed upper and lower front teeth. He had not given any significant medical, family, and dental history. Extra-oral examination ([Figure 1]) revealed good general health of patient with mesomorphic body type and he had a mesoprosopic facial form with good facial symmetry, convex profile with posterior divergence, reduced lower facial height, incompetent lips, obtuse nasolabial angle, deep mentolabial sulcus, low mandibular plane angle, and a non-consonant smile arc. No signs/ symptoms of temporomandibular joint dysfunction. On intra-oral examination ([Figure 2]) there was no abnormality detected in soft tissues. Good dental and periodontal health. Angle’s Class II division 2 malocclusion on both sides with Overjet of 1 mm and Overbite of 10 mm. Lower dental midline shifted toward right side by 1mm. No Cross bite or Scissor present. Exaggerated Curve of Spee. Examination of the lateral cephalometric radiograph ([Figure 3] and [Table 1]) indicated Retrognathic maxilla and mandible with ANB with skeletal Class II jaw bases. Patient had a normodivergent growth pattern on account of Sn-Go-Gn (30), FMA (26) and Jaraback ratio of 68%.

|
Measurements |
Pre treatment |
|
SNA |
79 º |
|
SNB |
72 º |
|
ANB |
7 º |
|
Beta Angle |
20º |
|
SN-GoGn |
30 º |
|
FMA |
26 º |
|
Jarabak ratio |
68% |
|
1 to NA |
0 mm |
|
1 to SN |
99º |
|
IMPA |
90 º |
|
Nasolabial Angle |
107 º |
|
Upper lip to E-Line |
-1 mm |
|
Lower lip to E-Line |
-2 mm |
Treatment objectives
Correction of the class II skeletal base
To improve profile and smile
To correct proclination of upper anteriors
To relieve crowding in lower arch
To achieve class I molar and canine relation on both sides
To reduce overjet
To correct deep bite
To establish functional occlusion
To ensure long-term stability
Treatment progress
After analysing all diagnostic records, the patient was treated without extractions. As he was in the pre-pubertal growth period, decompensation of the dental arches with leveling and aligning using the straight wire appliance (SWA). The maxillary teeth were bonded and banded with pre-adjusted 0.022” slot MBT prescription brackets. Initial levelling and alignment of maxillary arch was done. Brackets were bonded in the lower arch after sufficient overjet was achieved and the arches were aligned using the following sequence of archwires; 0.016 Niti, 17 × 25 Niti, and 19 × 25 Nickel Titanium arch wires. Later 19 × 25 stainless steel archwire ([Figure 5]) with exaggerated reverse curve of spee in the lower arch were placed to level and improve the torque of the incisors. After 9 months of treatment, both the arches were leveled and aligned.
The visual treatment objective (VTO) was positive showing improvement in facial esthetics when the mandible was advanced. So, the mandible was advanced to promote mandibular growth using the Forsus fatigue resistant appliance. The forsus fatigue resistant appliance ([Figure 7]) was fabricated and inserted followed by continuous activation by shims on the mandibular rod. This phase continued for 5 months. This resulted in forward positioning of mandible and mandibular incisors. Class II elastics has been given for prevention from relapse. Followed by finishing and detailing.


Treatment results
There was remarkable improvement in the patient’s profile and facial esthetics as seen in the post-treatment facial photographs. Facial balance, smile esthetics, and lip positions were improved. ([Figure 8]). There was intrusion and proclination of the upper and lower incisors. Class I molar and canine relationships were established. Overjet and overbite were improved to 0.5 and 2mm respectively ([Figure 9]). Cephalometrically the upper incisors were proclined from 0 mm to 3 mm in relation to NA perpendicular to point A line and lower incisors were proclined from 90 to 99 (IMPA) ([Table 2]). Superimposition demonstrated the treatment changes ([Figure 10]). There was a significant growth of mandible, mandibular molars were extruded and mesialized and mandibular anteriors showed proclination. In the maxillary arch there was extrusion of molar but no significant distalization and the incisors were proclined. There was a counter clockwise rotation of mandible, maxillary growth restriction, and overall improvement of soft tissue profile.



|
Measurements |
Pre treatment |
|
SNA |
79 º |
|
SNB |
73 º |
|
ANB |
6º |
|
Beta Angle |
26º |
|
SN-GoGn |
29 º |
|
FMA |
27 º |
|
Jarabak ratio |
70.3% |
|
1 to NA |
3 mm |
|
1 to SN |
97º |
|
IMPA |
99 º |
|
Nasolabial Angle |
100 º |
|
Upper lip to E-Line |
-1 mm |
|
Lower lip to E-Line |
0 mm |
Case-2
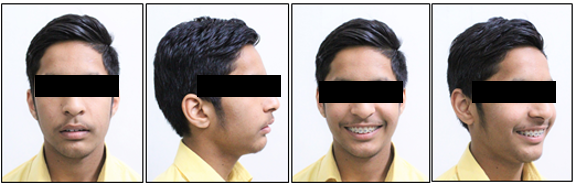
A 23 year old female patient reported to the department with chief complaint of irregularly placed upper and lower front teeth and impinging of teeth on tongue. She had not given any significant medical, family, and dental history. Extra-oral examination ([Figure 11]) revealed good general health of patient with mesomorphic body type and he had a mesoprosopic facial form with good facial symmetry, straight profile with straight divergence, reduced lower facial height, competent lips, normal nasolabial angle, normal mentolabial sulcus, low mandibular plane angle, and a non-consonant smile arc. No signs/ symptoms of temporomandibular joint dysfunction. On intra-oral examination ([Figure 12]) there was no abnormality detected in soft tissues. Good dental and periodontal health. Angle’s Class II (half cusp) division 2 malocclusion on both sides with Overjet of 3 mm and 100% Overbite. Concordant midline. No Cross bite or Scissor present. Exaggerated Curve of Spee. Examination of the lateral cephalometric radiograph ([Figure 13]) indicated orthognathic maxilla and mandible with skeletal Class I jaw bases. Patient had a hypodivergent growth pattern on account of Sn-Go-Gn (22),FMA (13) and Jaraback ratio of 72.4% ([Table 3]).



|
Measurements |
Pre treatment |
|
SNA |
76º |
|
SNB |
75º |
|
ANB |
1º |
|
Beta Angle |
29º |
|
SN-GoGn |
21º |
|
FMA |
13º |
|
Jarabak ratio |
72.4% |
|
1 to NA |
6 mm |
|
1 to SN |
97º |
|
IMPA |
96º |
|
Nasolabial Angle |
90º |
|
Upper lip to E-Line |
4 mm |
|
Lower lip to E-Line |
5 mm |
Treatment objectives
To correct the crowding of anterior teeth
Obtain optimum overjet and overbite
Establish Class I molar and canine relation
Obtain skeletal balance by restricting maxillary growth and promoting mandibular growth
Improve the facial features by obtaining a straight profile with straight divergence
Pleasing smile arc and soft tissue esthetics
Achieve good long term stability
Treatment progress
After analysing all diagnostic records, the patient was treated without extractions. Decompensation of the dental arches with leveling and aligning using the straight wire appliance (SWA). The maxillary teeth were bonded and banded with pre-adjusted 0.022” slot MBT prescription brackets. Initial levelling and alignment of maxillary arch was done. Brackets were bonded in the lower arch after sufficient overjet was achieved and the arches were aligned using the following sequence of archwires; 0.016 Niti, 17”×25” Niti, and 19”× 25” Nickel Titanium arch wires. Fixed anterior bite plane was inserted to relieve posterior teeth from occluding scissor bite lower left second pre-molar. Teeth 32 and 35 were aligned with the help of piggy back technique. Later 19”×25” stainless steel archire with palatal root torque in upper arch and labial root torque in lower arch to improve the torque of the incisors. After 13 months of treatment, both the arches were leveled and aligned ([Figure 14]).
The visual treatment objective (VTO) was positive showing improvement in facial esthetics when the mandible was advanced. The mandible was advanced to promote mandibular growth using the forsus fatigue resistance appliance. The forsus appliance ([Figure 15]) was fabricated and inserted followed by continuous activation by shims on the mandibular rod. This phase continued for 6 months. This resulted in forward positioning of mandible and mandibular incisors. Class II elastics were given for prevention from relapse.



Treatment results
There was remarkable improvement in the patient’s profile and facial esthetics as seen in the post-treatment facial photographs. Facial balance, smile esthetics, and lip positions were improved ([Figure 16]). There was intrusion and proclination of the upper and lower incisors. Class I molar and canine relationships were established. Overjet and overbite were improved to 0.5 and 2 mm respectively ([Figure 17]). Cephalometrically the upper incisors remained same 5 mm in relation to NA perpendicular to point A line and lower incisors were proclined from 96 to 108 (IMPA) ([Table 4]). Superimposition demonstrated the treatment changes ([Figure 18]). There was a significant growth of mandible, mandibular molars were extruded and mesialized and mandibular anteriors showed proclination. In the maxillary arch there was extrusion of molar but no significant distalization and the incisors were proclined. There was a counter clockwise rotation of mandible, maxillary growth restriction, and overall improvement of soft tissue profile.



|
Measurements |
Mid treatment |
|
SNA |
80º |
|
SNB |
78º |
|
ANB |
2º |
|
Beta Angle |
28º |
|
SN-GoGn |
22º |
|
FMA |
20º |
|
Jarabak ratio |
70% |
|
1 to NA |
5 mm |
|
1 to SN |
122º |
|
IMPA |
108º |
|
Nasolabial Angle |
75º |
|
Upper lip to E-Line |
5 mm |
|
Lower lip to E-Line |
6 mm |
Discussion
Lip competence, face convexity, dentoalveolar protrusion, skeletal discrepancy, dentoalveolar stability, and aesthetics must all be taken into account when considering a treatment for Class II malocclusion. In order to correct dentoalveolar protrusion or crowding, teeth must be extracted, and a retruded mandible requires either surgical advancement in the case of adults or therapy with any functional equipment for children. By applying specific fixed functional appliances, skeletal effects can be produced even during the deceleration phase of growth.
Treatment for young adults with Class II div 2 malocclusions after their peak velocity growth but with some residual growth is still possible using Fixed Functional Appliances. The hybrid fixed functional Forsus Fatigue Resistant Device comes in five different lengths: 25, 29, 32, 35, and 38 mm. In his master's thesis, Sood S. examined the cephalometric results in a group of seven patients and came to the conclusion that the Forsus FRD causes treated individuals to show a noticeable improvement in their profile, overjet, and overbite. The research revealed improvements in ANB angle, a significant increase in IMPA, and changes in mandibular length that are statistically significant.
For Class II malocclusions, FRD appliances are typically advised, particularly for patients who have mandibular dentoalveolar retrusion. In patients who are at or near the pinnacle of pubertal growth, this appliance can promote mandibular growth and advantageous dentoalveolar alterations. On the other hand, postpubertal patients typically have dental alterations. However, in this case report, the SNB angle increased by over 3 degrees, and the patient's forward mandibular displacement following therapy was only minor. This outcome is connected to the patient's limited residual growth throughout orthodontic treatment. The maxillary and mandibular arches showed signs of dentoalveolar alterations. Treatment with Forsus FRD in both instances resulted in the conversion of the Class II div 2 malocclusion to a Class I occlusion. Both skeletal and dentoalveolar parameters were improved by the treatment, but the ANB angle significantly improved in both cases. The most likely cause of this improvement was the unlocking of the mandible and its forward displacement following the correction of the retroclination of the maxillary incisors. The mandibular dentition moved forward, the mandibular incisors proclinated, and the maxillary incisors took on the appearance of headgear, all of which helped correct the overjet. Utilising the patient's residual growth as a benefit allowed for the avoidance of orthognathic surgery, and employing fixed functional therapy in conjunction with fixed orthodontic treatment allowed for the completion of the treatment in a single phase, cutting down on treatment time. Patient compliance was also not a problem.from a Class I occlusion to a malocclusion.
Jones G, Buschang PH, Kim KB and Oliver DR (2008) [10] evaluation of Forsus Fatigue Resistant Device (FRD) as a compliance-free alternative to Class II elastics showed significantly greater lower molar mesial movements and total molar correction in the Forsus group with a general trend for mesial movement of the maxilla, mandible, and dentition during treatment for both groups. [11] The mandibular skeletal advancement and dental movements were greater than those in the maxilla, which accounted for the Class II correction. Lower incisor proclination was evident in both groups. Vertically, the maxillary and mandibular molars erupted during treatment in both groups, while lower incisors proclined. Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E and Baccetti T (2011) [8] concluded that Forsus Fatigue Resistant Device in Class II patients with the help of lateral cephalograms showed a significant restraint in the sagittal skeletal position of the maxilla (also at the soft tissue level), a significant increase in mandibular length, and a significant improvement in maxillo-mandibular sagittal skeletal relationships, significant reduction in overjet and a significant increase in molar relationship. The lower incisors were significantly proclined and intruded, while the lower first molars moved significantly in a mesial and vertical direction. It led to the conclusion that the FRD protocol is effective in correcting Class II malocclusion with a combination of skeletal (mainly maxillary) and dentoalveolar (mainly mandibular) modifications. Sood S, Kharbanda OP, Duggal R, Sood M, Gulati S (2011)[12], [13] had done a study on Class II division 1 malocclusion, there was a significant decrease in the muscle activity at one month after Forsus Fatigue Resistant Device insertion during swallowing of saliva and maximal voluntary clenching which gradually returned to pre-treatment levels at the end of six months. G. Bhavani, R. Navaneethan (2017) [14] suggested that significant skeletal changes commonly seen are the restriction of the maxillary growth and the increase in mandibular length. However, the restriction of the maxillary growth is more predominant than that of the increase in mandibular length. The most significant changes in the mandible are more dentoalveolar than the skeletal. Amal I. Linjawi and Mona A. Abbassy (2018) [15] concluded that Forsus appliance showed the following dentoalveolar effects: protruding, proclining, and intruding lower incisors, retroclining upper incisors, distalizing, and intruding upper molars, as well as reducing overjet and overbite. Stefanos Matthaios, Apostolos I. Tsolakis, Anna-Bettina Haidich, Ioannis Galanis and Ioannis A. Tsolakis (2022) [16] compared Forsus appliance to Class II elastics, Forsus has equivalent dental effects to Class II elastics, but it is more effective in molar correction, overjet reduction, and controlling of the upper incisor inclination.
Conclusion
The little growth that was still present in the patient was utilised to successfully correct the sagittal discrepancy of the jaws with a fixed functional device. Finally, it can be said that when used in conjunction with a fully bonded fixed appliance, fixed functional appliances in general and the Forsus fatigue resistant appliance in particular make it easier to repair Class II Div 2 malocclusions while also shortening the treatment's length. The skeletal alterations that include a headgear-like impact on the maxilla, distalization of the maxillary molars, mesialization of the mandibular molars, and proclination of the mandibular incisors are the main contributors to the improvement.
Source of Funding
None.
Conflict of Interest
None.
References
- WR Proffit, HW Fields, LJ Moray. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES-III survey. Int J Adult Orthodon Orthognath Surg 1998. [Google Scholar]
- C Nelson, M Harkness, P Herbison. Mandibular changes during functional appliance treatment. Am J Orthod Dentofac Orthop 1993. [Google Scholar]
- P Cozza, T Baccetti, L Franchi, L De Toffol, JA Mcnamara. Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop 2006. [Google Scholar] [Crossref]
- L Franchi, L Alvetro, V Giuntini, C Masucci, E Defraia, T Baccetti. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in Class II patients. Angle Orthod 2011. [Google Scholar]
- N Ahmed, VN Aravinda, R Joseph, KRR Bhat, A Younus. Combination of forsus fatigue resistant device and premolar extraction for the management of a skeletal class II malocclusion. IP Indian J Orthod Dentofacial Res 2021. [Google Scholar]
- S Sood, O P Kharbanda, R Duggal, M Sood, S Gulati. Muscle response during treatment of Class II Div 1 malocclusion with Forsus Fatigue resistant device. J Clin Pediatr Dent 2011. [Google Scholar]
- AK Ritto. The Forsus Fatigue Resistant Device. J Clin Orthod 2006. [Google Scholar]
- L Franchi, L Alvetro, V Giuntini, C Masucci, E Defraia, T Baccetti. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device n Class II patients. Angle Orthod 2011. [Google Scholar]
- MM El - Sheikh, K Godfrey, M Manosudprasit, N Viwattanatipa. Force deflection characteristics of the fatigue-resistant device spring : an in vitro study. World J Orthod 2007. [Google Scholar]
- G Jones, P H Buschang, K B Kim, Oliver Dr. Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod 2008. [Google Scholar]
- A Aras, Ada E Saracoglu, H Gezer, NS Aras, I. Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop 2011. [Google Scholar]
- S Sood, O P Kharbanda, R Duggal, M Sood, S Gulati. Muscle response during treatment of Class II division I malocclusion with Forsus Fatigue Resitant Device. J Clin Pediatr Dent 2011. [Google Scholar]
- BC Karunakara, GS Shwetha. Precise insertion of the Forsus Fatigue Resistant Device. Jclin Orthod 2010. [Google Scholar]
- G Bhavani, R Navaneethan. Forsus Appliance - A Review. Res J Pharmd Tech 2017. [Google Scholar]
- A I Linjawi, MA Abbassy. Dentoskeletal effects of the forsus™ fatigue resistance device in the treatment of class II malocclusion: A systematic review and meta-analysis. J Orthod Sci 2018. [Google Scholar] [Crossref]
- S Matthaios, A I Tsolakis, A.-B Haidich, I Galanis. Tsolakis, I.A. Dental and Skeletal Effects of Herbst Appliance, Forsus Fatigue Resistance Device, and Class II Elastics-A Systematic Review and Meta-Analysis. J Clin Med . [Google Scholar] [Crossref]
