Introduction
The occurrence of irregularities or malformations can occur in the dentition, such as abnormal number, eruption, morphology and position of teeth. Hyperdontia or the presence of supernumerary teeth can be defined as the presence of excess tooth substance or tooth in the oral cavity. Supernumerary teeth may be single or multiple, unilateral or bilateral, and erupted or impacted.1 They are more commonly observed in the maxilla as compared to the mandible and occur more frequently in the incisal than in the molar region. 2 Depending on their location in the dental arches, supernumerary teeth can be categorized into mesiodens, parapremolar, paramolar and distomolar; and based on their morphology, they are classified as rudimentary or supplemental.3, 4 The incidence of supernumerary teeth varies between 0.1% to 3.8% in permanent dentition and between 0.3% to 0.6 % in primary dentition. Asian population has been reported to exhibit the highest incidence of supernumerary teeth.1 There is ambiguity in the literature regarding the etiopathogenesis of this anomaly ranging from genetic, atavistic, vascular and dental lamina hyperfunction, the latter being by far the most accepted.5 A distomolar also known as dens distomolar, retromolar or fourth molar is a supernumerary tooth present distal or posterior to the third molar. Distomolars can be fully erupted or impacted with their ratio being 1:5 as stated in past literature. 5 Undiscovered distomolars have been rarely reported to cause any complications within the oral cavity.6 But in certain cases, they may lead to odontogenic inflammation, cystic lesions, periodontal issues and neuralgic pain. 5
Impact of high altitude on the stmotognathic system
Chronic exposure to high altitude and hypoxia leads to an increase in inflammatory markers, as there is a greater amount of oxidative stress as well as lower systemic and local anti-oxidant capacity, which is known to have a deleterious effect on the stomatognathic system and oral health. These mechanisms eventually lead to increased alveolar bone loss, altered periodontal ligament height, decreased salivary flow and may significantly increase the incidence of pericoronitis.7 Hypoxia, especially in chronic cases, has been known to lead to stress erythrocytosis, resulting in increased load on organs such as the liver, spleen and kidneys to help in the regulation of the optimal level of RBCs and myeloid cells in order to combat hypoxia and inflammatory markers. In the initial stages, this causes the haemoglobin levels to rise up to or more than 19 G/dL in females and 21 G/dL in males. Ultimately, it leads to more inflammation and stress anaemia in certain individuals.8 These are the major factors to be considered while performing oral surgical procedures at high altitude. We present the case of a symptomatic mandibular distomolar and its management at a remote dental centre setup located in Ladakh at altitude of 14500 ft above mean sea level.
Case Report
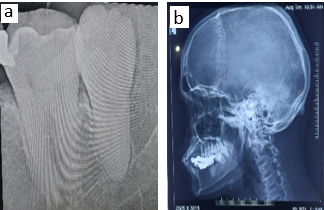
A 28-year-old male patient reported to the dental section of a field hospital situated in Tangtse, a remote high-altitude location situated at approximately 14500 feet above mean sea level in Ladakh. He ‘presented with acute severe pain' in the left lower back region of his mouth. He had an intermittent history of similar but milder pain for last 3 months. Intraoral examination revealed the presence of a fully erupted mandibular left third molar with fixed prosthesis present in respect to the left mandibular first molar, second molar and second premolar. The tissue distal to the third molar showed signs of inflammation (Figure 1 ) and an intraoral periapical radiograph was recorded which revealed a fully formed impacted distomolar (Figure 2a). Since an orthopantomogram was not available in the facility, a left lateral view of the skull was recorded to appreciate the presence of the distomolar and record its relation to the surrounding tissues (Figure 2b). The distomolar showed complete development and was vertically impacted distal to the third molar. Based on the clinical and radiological features, the diagnosis of perocoronitis in respect to the impacted left mandibular distomolar was made. After conducting routine hematological investigations and recording the patient’s consent, he was given clearance to undergo the procedure to remove the offending tooth. The patient was put on antibiotic cover and surgical extraction of the impacted distomolar was planned. Under strict aseptic conditions, inferior alveolar nerve block and long buccal nerve block were administered using 2% lignocaine HCl with 1:80000 adrenaline (Triocaine Plus). Modified Ward’s incision was given using No. 15 Bard Parker blade and a mucoperiosteal flap was raised. Following this, buccal bone guttering was done using straight carbide bur (Prima Classic HP 701) at 45,000 RPM under copious saline irrigation and the tooth was delivered in-toto using a Coupland elevator. Post extraction, the socket was inspected for any remaining bone or tissue fragments and irrigated with normal saline after which, the flap was approximated using two interrupted 3-0 silk sutures (Lotus Silkus). The procedure took place uneventfully and there were no complications during or after the surgery (Figure 3, Figure 4, Figure 5, Figure 6, Figure 7). The patient was kept on regular follow-up for the following four weeks and the extraction socket healed satisfactorily with no associated post-surgical complications.
Discussion
A distomolar is a supernumerary tooth found distal to the third molars, either following the line of arch or slightly offset to it. The incidence of distomolars has been reported to vary from 0.3% to 2.1%. The maxilla has been noted to have a higher incidence of distomolars than the mandible. 9, 10, 11 The higher prevalence in males has been postulated to be associated with the autosomal recessive gene, which has greater penetration in males. 12 Distomolars are usually asymptomatic but if impacted, they may result in infection, pain, cystic lesions, root resorption and pulpal necrosis of the adjacent tooth as well as neuralgia of the trigeminal nerve. Erupted distomolars may cause malocclusion, delayed or ectopic eruption of adjacent teeth, periodontal disease, traumatic bite and caries. 13, 14 Clinical and radiographic evaluation are the key factors in diagnosing distomolars. Radiographic assessment is the most definite method for the diagnosis of unerupted distomolars. The most commonly used radiographs are panoramic, occlusal and periapical, with the panoramic radiograph being the most valuable diagnostic tool. New advancements such as cone beam computed tomography (CBCT) are more specific and have proven to be quite beneficial in detecting the accurate location of these anomalies along with their relation to the surrounding structures. 15 It may be difficult to come up with a single ideal treatment protocol for the management of distomolars. The treatment plan depends on the location of the supernumerary tooth as well as its potentially deleterious effects on the surrounding hard and soft tissues. Such teeth may be kept under observation if there are no associated symptoms, however, extraction is indicated in case of the presence of any of the aforementioned complications. In the present case, there were various clinical as well as physiological challenges involved in its management at such a remote location. Difficult terrain in addition to service exigency did not permit for timely referral of the patient to a higher center. The surgery had to be performed in an emergency with limited equipment as the patient was in excruciating pain and had already taken multiple courses of antibiotics and analgesics. It has been observed that in addition to hypoxia, high altitude leads to an increase in inflammatory markers, leading to delayed healing. This, in addition to increased hemoglobin levels and transient hypertension, poses a major physiological challenge while performing surgical procedures. Despite all these challenges, our patient underwent the procedure uneventfully and had remarkable recovery in the post procedure period.
Conclusion
High altitude, which the Indian Army defines as an altitude above 2700m (9000 feet), alters the normal physiological response of the human body. This results in an increase in inflammatory markers, raised hemoglobin levels and transient hypertension which, when coupled with the associated hypoxic environment, has been observed to cause a delay in the normal healing process. This scenario poses a major challenge for the dental surgeon to perform surgical procedures at high altitude areas.