- Visibility 212 Views
- Downloads 30 Downloads
- Permissions
- DOI 10.18231/j.ijohd.2022.002
-
CrossMark
- Citation
Zygomatic implants– Changing face of implant dentistry
Abstract
Conventional implants cannot be placed in patients with severe atrophied maxilla resulting in insufficient amount of bone remaining for anchorage. Routinely, grafts were the preferred technique. But the drawbacks associated with this procedure, Branemark proposed surgical /prosthetic rehabilitation with zygomatic implants to overcome them. This review aims to address the criteria for placement, surgical and prosthodontics procedure, outcome evaluation and complications arising with zygomatic implants.
Introduction
Literature evidence documents the success of implant supported prosthesis in addressing edentulousness. But, the extension of this to maxillary intervention is questionable due to atrophy of bone and pneumatization of maxillary sinus.[1], [2] Various alternative techniques are practiced such as composite graft placement,[3] Le Fort I osteotomy,[4] grafts in iliac crest and maxillary sinus.[5], [6]
But these choices further lengthen the treatment duration, might call for hospitalization and makes it impossible to use provisional prosthesis in healing phase. Additionally, the grafts in the donor sites are prone for sensitivity problems, hematomas and hyperalgesia. The adoption of a two stage procedure with delayed placement of implant further increases the patient discomfort.[7]
A feasible alternative for treating individuals reporting with severely atrophied maxilla is considering the zygomatic bone as an anchorage for implant placement as proposed by Prof. Branemark in 1988,[8] who used it for prosthetic rehabilitation in hemimaxillectomy individuals. The successful outcome of these implants in terms of acceptance and long term stability made Branemark develop the zygomatic implant even when the maxillary conditions were unfavourable. This novel technique offered an alternative to invasive procedures such as bone grafting and sinus lifting.
Zygomatic Implant
Zygomatic fixtures are inserted into the maxillary second premolar region of the resorbed ridge in the palatal side, via the maxilla sinus into the zygomatic compact bone. It is available in varying lengths of 35 to 52.5 mm and encompasses a 458 angulated head to recoup for the angulation between zygoma and maxilla. The thickness of the implant is around 4 mm in the zygomatic region while it is 4.5 mm near the alveolar process. The angulation in the platform extremity allows for fixing any type of abutment from the Branemark system. The placement of two to four additional implants placed in the premaxilla provides for the adoption of a hybrid fixed prosthesis, which creates a stable biomechanical polygon.[9]

Pre-surgical Evaluation and Prosthetic Guidelines for Zygomatic Graft Placement
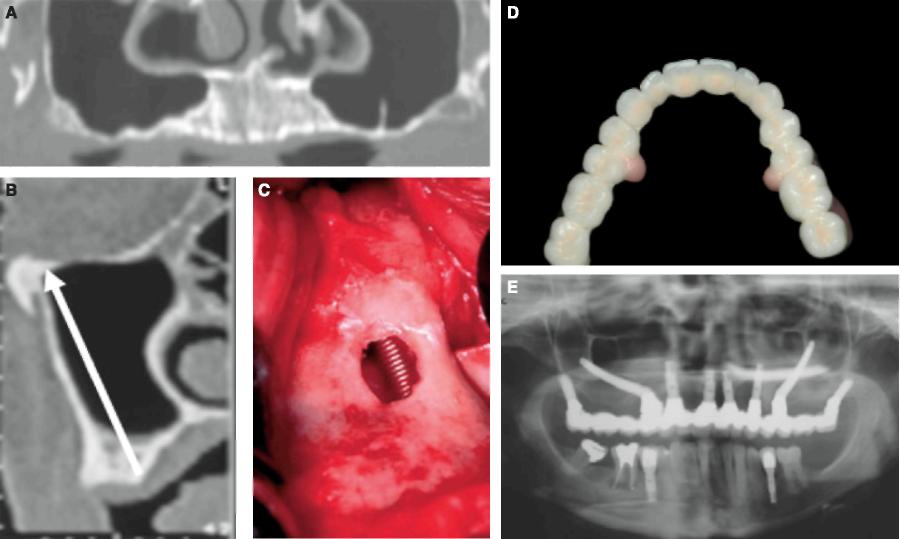
Pre – surgical evaluation: Implant insertion through the maxillary sinus and zygoma poses a significant challenge. Level of maxilla, sinus and zygoma are to be evaluated, both clinically and radiologically. Because OPG can produce inaccurate information, the spiral or helicod computed tomography (CT) scan, which allows for two- and three-dimensional imaging, is the preferred assessment. In addition, The CT scan checks on the health of the maxilla and sinuses. Sinusitis, polyps, and any other sinus pathology can be ruled out. The zygoma's density, length, and volume can be assessed, and unique templates for putting the zygomatic implants can be created on stereolithographic models to simplify zygomatic implant orientation during surgery with minimal angulation and position mistakes. A software is provided by Oralim (Medicim, Leuven), wherein implants are placed via virtual images and the dentist merely needs to convert the images to clinical situation's reality.[10]
Prosthetic guidelines
When using the Zygomatic implant, general prosthetic design recommendations must look into;
Incorporation of sufficient rigidity and precision while restoring to reduce bending moments.
Promote maintenance by balancing functional, aesthetic, phonetic, and hygiene needs.
If the prosthesis is not stiff enough, the zygoma implant can bend and deflect, resulting in implant failure or screws loosening.
Surgical Procedure of Zygomatic Implant
Implant surgery is generally done under general anesthesia. Local anesthetic agent is infiltrated in the maxillary vestibular region of the zygoma, 1 cm palatal to crestal bone. A mid crestal incision with vertical releasing incisions in the posterior region of infrazygomatic crest in front of the surgical location is made to expose the area. The first landmark, anterior border of the zygomatic arch is then marked. Lateral border of the orbit forms the second landmark. Subsequently, mucoperiosteal flap is elevated to expose the central or the posterior region of the zygomatic arch. Any obtrusion with orbit, lateral border of the maxillary sinus and alveolar crest is avoided, by positioning a retractor.
Bone windows of approximately 10 mm wide are made on the lateral border of maxillary sinus along with desired path of zygomatic fixature. The drilling direction considers the biomechanics of future rehabilitation and prosthetic design as seen in [Figure 2]. Zygomatic bone and alveolar bone are drilled to accommodate the estimated implant length. By using a motor or a fixture mount, the self-tapping implant is inserted, with caution to not expand the palatal hole, particularly if it thin alveolar or basal bone. Bone fragments collected locally can be placed around the zygomaticus implant if necessary. The implant is secured with a cover screw, and the mucoperiosteal flap is sutured. The abutment connection is fixed 6 months later with the help of a straight or regular angulated multiple – uit Branemark abutment.
Prosthetic Procedure
Prosthesis placement is as per the conventional guidelines laid down for implant supported dental bridges (either cemented or screw based). The design of the bridge must articulate enough to maintain hygiene around the area as the zygomatic implants are placed 10 -15 mm towards the medial side of the ridge.
Implant Design
The conventional Branemark zygomatic fixture was intended to be placed via the maxillary sinus into the zygomatic compact bone from the palatal side of the resorbed maxilla in the vicinity of the second premolar. It exhibited the features of a traditional implant at first, but it was longer and wider. The implant was made of titanium, of self tapping type with a assembled surface ranging in lengths of 30 to 52.5 mm. The threaded apical part was 4 mm in diameter, and the crestal part was 4.5 mm in diameter. An inner thread was added to the implant head to allow standard abutments to be connected. The head was later angulated to 45 degrees. The surface has refined to a roughened oxidised threaded surface in today's installation, and the head now incorporates an implant driver screw that stays inside the implant, providing an inner thread for the connection of 'zygomatic' abutments. [11]
Evolution of Zygomatic Implants
The introduction of zygomatic implants for rehabilitating patients with compromised maxillary bone structure initiated a new phase of implant dentistry. The initial procedure as putforth by Branemark practice a vestibular incision, simulating a LeFort I incision, with periosteal elevation followed by anthrotomy. [1] But the palatal drift of implant posed a non favourable position of the palate resulting in problems with phonetics, hygiene and comfort.
To overcome this Stella and Warner modified Branemark’s technique by embedding the implant within the maxillary sinus. Slots were prepared on the exterior surface of sinus, thus addressing the implant head position.[12]
Clinical Outcome
Literature upholds a higher success rate of zygomatic implants, irrespective of the position or technique. Bedrossian et al[13] reported a 100% success rate for 80 implants placed conventionally and 44 within the sinus. In a study done in 2004, Hirsch et al[14] demonstrated a survival rate of 97.9% after 12 months follow up. The authors also looked for satisfaction component and found that 80% of them were content with the functional and esthetic outcome. Malo et al[15] reported 98.8% success rate in 92 immediately loaded zygomatic implants following a 5 year follow up. In a systematic review compiled by Candel-Marti et al,[16] immediate loaded implants had a success rate of 96.37% -100% and late loading implant (3 – 6 months later) showed a success rate of 89 – 100%. The overall mean success rate was reported to be 97.05%.
Zygomatic Stability
Varying levels of implant stability could be observed due to the particular biomechanics of extra-maxillary positioned zygomatic implants, wherein little or none anchorage is achieved at the head height. When implants placed in the extra sinus region are evaluated separately, modest movement with no other related clinical symptoms may be identified. The anchoring zygomatic bone has an elastic modulus that allows it to bend when a force is applied remotely. The rotational movement must be avoided, and it will be eliminated once the implants are splinted up. Rotational movement must be regarded as an indication of implant failure. [11]
Post operative Complications
Zygomatic implants poses the risk of rhinosinusitis. Any patient with probable risk for developing rhinosinusitis must be recognized and consulted with a otolarygologist prior to placement of zygomatic implants. Certain longitudinal studies have reported incidence of soft tissue dehiscences.
Recent Developments of the Zygomatic Fixture Technique
Immediate loading
Immediate loading helps patients to have a joint surgical/prosthetic therapy without having to wait for osseointegration to occur, enabling masticatory function to resume with a fixed implant-supported complete denture. Despite the fact that clinical reports of immediately loaded implants are few in literature the results were positive. The use of ZIs in immediate functionality is especially promising, because the rigid splinting of inclined implants dissipates axial and lateral loads, stabilising the rehabilitation system. Duarte L R et al[17] evaluated a different surgical / prosthetic approach to treat severely atrophied maxilla with four zygomatic implants by immediate loading. Osseointegration was achieved in 47 of 48 ZIs and sinus pathology was detected in none.
Only 1 implants did not attain osseointegration.
ZIs inserted, one implant failed to achieve osseointegration. The prosthetic parts functioned properly with no sinus pathologies found in any of the treated individuals.
Placement under local anesthesia:
ZI is recommended to be placed under local anesthesia when the procedure can be completed within 1.5 hours under an experienced dental surgeon. The procedure employs four different approaches to be applied simultaneously.
Lidocaine with epinephrine infiltration anaesthesia in the buccal sulcus from the central incisor to the third molar teeth (about 3.6 ml), 1 cm palatal to the bone crest, block of the posterior superior alveolar nerve.
Infra-orbital nerve block using lidocaine with epinephrine or felypressine with around 1.8 ml of prilocaine administered orally.
lidocaine with epinephrine or felypressine with around 1.8 ml of prilocaine to occlude the spheno-palatine ganglion traversing the larger palatine foramen.
3.6 mL lidocaine with epinephrine infusion anaesthetic over the zygoma area through the skin.
Multiple zygomatic implants
Bothur et al[18] used a modified zygomatic implant procedure, which involves placing up to three implants to every side of the maxilla to anchor a dental prosthesis. The posterior most implant is placed in the second molar region, the second in the premolar and third in the lateral incisor region and the drill used are longer by 50mm as compared to the conventional technique.
Extra sinus placement
In individuals with significant buccal concavities on the lateral side of the maxillary sinus, zygomatic prosthesis implantation via an intrasinus channel may be challenging. As a result, an extrasinus method for placement is established, with the implant head emergence occurring at or in proximity to the top of remnant alveolar crest, often in the second premolar to first molar area. Furthermore, upon accessing the zygomatic bone, the implant bodies should ideally engage the lateral bone wall of the maxillary sinus. The implant area is prepped without cutting a hole in the maxillary sinus, and typical zygomatic implant drilling stages are followed.
Conclusion
Zygomatic implant helps to surgically rehabilitate patients with severe maxillary resorption and also presents with higher acceptance rate of treatment because of immediate use of dentures. Zygomatic implants have recognized as having better clinical results than bone grafting and may be the new "gold standard" therapy for conceding maxillary bone. It has been in use for over a decade and provides a consistent outcome in the rehabilitation of individuals who are completely or partially edentulous. Further studies of prospective nature are advocated.
Conflict of Interest
None.
References
- Brånemark P, Gröndahl K, Ohrnell L, Nilsson P, Petruson B, Svensson B. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70-85. [Google Scholar]
- Rigolizzo M, Camilli J, Francischone C, Padovani C, Brånemark P. Zygomatic bone: anatomic bases for osseointegrated implant anchorage. Int J Oral Maxillofac Implants. 2005;20(3):441-7. [Google Scholar]
- Breine U, Brånemark P. Reconstruction of alveolar jawbone. An experimental and clinical study of immediate and preformed autologous bone grafts in combination with osseointegrated implants. Scand J Plast Reconstr Surg. 1980;14(1):23-48. [Google Scholar]
- Isaksson S, Ekfeldt A, Alberius P, Blomqvist J. Early results from reconstruction of severely atrophic (class VI) maxillas by immediate endosseous implants in conjunction with bone grafting and Le Fort I osteotomy. Int J Oral Maxillofac Surg. 1993;22(3):144-8. [Google Scholar]
- Isaksson S, Alberius P. Maxillary alveolar ridge augmentation with onlay bone grafts and immediate endosseous implants. J Craniomaxillofac Surg. 1992;20(1):2-7. [Google Scholar]
- Wood R, Moore D. Grafting of the maxillary sinus with intraorally harvested autogenous bone prior to implant placement. Int J Oral Maxillofac Implants. 1988;3(3):209-14. [Google Scholar]
- Nkenke E, Hahn M, Lell M, Wiltfang J, Mosgau SS, Stech B. Anatomic site evaluation of the zygomatic bone for dental implant placement Clin. Clin Oral Implants Res. 2003;14(1):72-9. [Google Scholar]
- Darle C. Minimized treatment for maximal predictability: a new procedure for rehabilitating the severely resorbed maxilla. Talk of the times 4. 1999. [Google Scholar]
- Malevez C, Daelemans P, PA, Durdu F. Use of zygomatic implants to deal with resorbed posterior maxillae. Periodontol 2000. 2003;33:82-9. [Google Scholar]
- Steenberghe D, Malevez C, Cleynenbreugel J, Serhal C, Dhoore E, Schutyser, F. Accuracy of drilling guides for transfer from three-dimensional CT-based planning to placement of zygoma implants in human cadavers. Clin Oral Implants Res. 2003;14(1):131-6. [Google Scholar]
- Aparicio C, Manresa C, Francisco K, Claros P, Aliandez J, González-Martín O. Zygomatic implants: indications, techniques and outcomes, and the Zygomatic Success Code. Periodontol 2000. 2000;66(1):41-58. [Google Scholar]
- Stella J, Warner M. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: A technical note. Int J Oral Maxillofac Implants. 2000;15(6):889-93. [Google Scholar]
- Bedrossian E, Stumpel L, Beckely M, Indresano T. The zygomatic implant: preliminary data on treatment of severely resorbed maxillae. A clinical report. Int J Oral Maxillofac Implants. 2002;17(6):861-5. [Google Scholar]
- Hirsch J, Ohrnell L, Henry P, Andreasson L, Brånemark P. A clinical evaluation of the Zygoma fixture: One year of follow-up at 16 clinics. J Oral Maxillofac Surg. 2004;62(9 Suppl):22-9. [Google Scholar]
- Maló P, Nobre M, Lopes A, Ferro A, Moss S. Five-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded zygomatic implants placed extra-maxillary. Eur J Oral Implantol. 2014;7(3):267-81. [Google Scholar]
- Candel-Martí E, Carrillo-García C, Peñarrocha-Oltra D, Peñarrocha-Diago M. Rehabilitation of atrophic posterior maxilla with zygomatic implants: review. J Oral Implantol. 2012;38(5):653-7. [Google Scholar]
- Duarte L, Filho H, Francischone C, Peredo L, Brånemark P. The establishment of a protocol for the total rehabilitation of atrophic maxillae employing four zygomatic fixtures in an immediate loading system--a 30-month clinical and radiographic follow-up. Clin Implant Dent Relat Res. 2007;9(4):186-96. [Google Scholar]
- Bothur S, Jonsson G, Sandahl L. Modified technique using multiple zygomatic implants in reconstruction of the atrophic maxilla: a technical note. Int J Oral Maxillofac Implants. 2003;18(6):902-4. [Google Scholar]
- Abstract
- Introduction
- Zygomatic Implant
- Pre-surgical Evaluation and Prosthetic Guidelines for Zygomatic Graft Placement
- Surgical Procedure of Zygomatic Implant
- Prosthetic Procedure
- Implant Design
- Evolution of Zygomatic Implants
- Clinical Outcome
- Zygomatic Stability
- Post operative Complications
- Recent Developments of the Zygomatic Fixture Technique
- Conclusion
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Aeran H, Singh G, Seth J, Agarwal A. Zygomatic implants– Changing face of implant dentistry [Internet]. Int J Oral Health Dent. 2022 [cited 2025 Sep 14];8(1):5-8. Available from: https://doi.org/10.18231/j.ijohd.2022.002
APA
Aeran, H., Singh, G., Seth, J., Agarwal, A. (2022). Zygomatic implants– Changing face of implant dentistry. Int J Oral Health Dent, 8(1), 5-8. https://doi.org/10.18231/j.ijohd.2022.002
MLA
Aeran, Himanshu, Singh, Gaurav, Seth, Jyotsna, Agarwal, Anubha. "Zygomatic implants– Changing face of implant dentistry." Int J Oral Health Dent, vol. 8, no. 1, 2022, pp. 5-8. https://doi.org/10.18231/j.ijohd.2022.002
Chicago
Aeran, H., Singh, G., Seth, J., Agarwal, A.. "Zygomatic implants– Changing face of implant dentistry." Int J Oral Health Dent 8, no. 1 (2022): 5-8. https://doi.org/10.18231/j.ijohd.2022.002
