Introduction
Papillon-Lefèvre syndrome (PLS) is a very rare genodermatosis of autosomal-recessive inheritance. It is an ectodermal dysplasia, and a type IV palmoplantar keratosis.1, 2, 3 Palmoplantar keratoderma refers to a heterogeneous group of disorders characterized by thickening of the palms and soles, which can be hereditary, acquired, or associated with syndromes.4, 5 In 1924, two French physicians Papillon and Lefevre described a brother and sister with a condition characterized by palmoplantar hyperkeratosis associated with severe, early onset periodontitis and premature loss of primary and permanent teeth.5, 6
The etiology of PLS is multifactorial with genetic, immunological, and microbial factors playing a role in etiopathogenesis. Recently identified genetic defect in PLS has been mapped to chromosome11q14–q21, which involves mutations of cathepsin C (CTSC).1, 2, 4, 5, 6, 7 This involved in a wide variety of immune and inflammatory responses by activating serine proteinases expressed in the granules of bone marrow-derived cells from both the myeloid and lymphoid series. This loss of CTSC function and subsequent inactivity of neutrophil serine proteinases may cause deregulation of localized polymorphonuclears response in inflamed periodontal tissues, leading to the severe tissue destruction in PLS.7, 8 Aggregatibacter actinomycetemcomitans was reported to have a significant role in the progression of periodontal involvements. Other microbial agents including Porphyromonas gingivalis, Fusobacterium nucleatum, and Treponema denticola have also been suggested to have causal effects.4, 5, 6, 7, 8
This disease usually has its onset between the ages of 1 to 4 affecting males and females equally. Its prevalence estimated to be 1 to 4 per million in general population with carrier rate of 2 to 4 per 1000. It is known that consanguineous marriages may lead to an increased expression of autosomal recessive disorders in 20 to 40% of patients with PLS.2
Dermatological disorders initiate with erythema and after about 6 months, they progress to hyperkeratosis of soles of feet and palms of hands (palmer-plantar). This exacerbates in winter, leading to painful fissures.2 Oral manifestation involves extensive, severe, aggressive and prepubertal periodontitis, leading to premature loss in both deciduous and permanent dentitions without any signs of root resorption. Hypermobility, drifting and migration is also seen.1, 2, 4, 5, 6, 7 Both maxillary and mandibular alveolar ridges are highly resorbed resulting in reduced vertical dimension of occlusion and, hence, the patient will have characteristic “denture face” appearance.7 Other less frequently reported features include psoriasiform plaques of the elbows and knees, nail changes, calcification of the dura, and recurrent pyogenic skin infections.5, 6, 7 A well-documented case series of PLS among three siblings of first cousin married parents is presented. The oral and cutaneous manifestations and current treatment modalities are discussed.
Presentation of cases
All Three siblings a 11-year-old male, a 9-year-old female and a 7-year-old male came to department of oral medicine and radiology with chief complaint of pain, mobility and multiple missing teeth in oral cavity since childhood. Patients were relatively asymptomatic before 2 – 3 years of birth then they experienced thickening of palm and sole skin with fissuring Figure 1 and early self-exfoliation of teeth due to mobility Figure 2, but they didn’t take any treatment regarding these symptoms. They visited to a private clinic from where they were referred for needful treatment.
Past dental history reveals normal eruption of deciduous and permanent teeth and early self-exfoliation of deciduous and permanent teeth in all three cases and no any relevant medical history. There was no family history of ichthyosis or hereditary or acquired palmoplanter keratodermas. All siblings were affected but parents were normal and parents had history of consanguineous marriage as they were first cousins.
All findings related to PLS of affected siblings is describe in false .
Figure 1
Showing skin manifestations- (A) CASE 1 showing absenceof keratotic lesionson elbow. (B) and (C) presentsCASE 2 and CASE 3respectively showing well-demarcated, yellow keratotic lesion with scales andfissuring on soles and palms.

Figure 2
Shows intraoral pictures of case 1, 2 and 3 in (A), (B) & (C)respectively. It showing missing permanent teeth, gingival recession andperiodontitis.

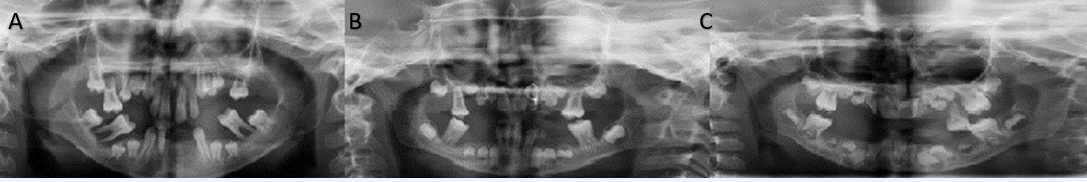
Figure 3
OPG IMAGES showing CASE 1, CASE 2 and CASE 3 in (A), Band (C) generalized severe loss of PDL with horizontal and vertical bone loss leading to decrease in height of alveolar bone. Also, note migration and floating tooth appearance.
Other investigations
Due to their young age and lack of cooperation IOPAs were not taken. OPG showed loss of supporting periodontium up to apical third of root apex and arc shaped severe resorption of alveolar bone around the remaining teeth giving floating-in-air appearances. There was more vertical bone loss than horizontal bone loss. Decrease in height of alveolar bone. And also missing multiple permanent teeth, all showed in Figure 3. On lateral cephalogram and PA skull, there was no evidence of intracranial calcification in all patients in Figure 4. CT scan view is also shown Figure 5.
Laboratory investigations was carried out, which included hematological and biochemical investigations. Routine blood investigations showed reduced Hb and hematocrit values. While differential counts were increased in all cases. All other investigations were normal.
In all three cases based on the history, clinical examination, and radiographic examination, a provisional diagnosis of papillon-lefevre syndrome was made.
Table 1
Case presentation- Patient details and clinical findings
Discussions
PLS is a rare disorder, it is inherited in an autosomal recessive manner, in which both parents are phenotypically healthy and there is no family history of the disease, other than the affected person and possibly some siblings. Both parents must carry the autosomal gene for the syndrome to appear in their offspring. When 2 such carriers mate, there is a 25% chance of producing affected offspring.2, 4, 5 Most of the cases reported so far two siblings affected1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 3 except for a few cases in which three or more siblings affected.4, 5, 6, 7, 8, 9, 10, 11, 12, 3, 13 in our case three siblings are affected which is a rare condition.
Consanguineous marriage is matrimony between persons who are closely related. It is defined as a union between two individuals who are related as first or second cousins or closer. Increased genetic risks to the offspring represent main negative impact of consanguineous marriage, as it may lead to increased expression of autosomal recessive disorders.1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 3, 13, 14 In our case patient’s parents had consanguineous marriage which results in affecting all siblings.
The pathogenesis of PLS involve mutations of the cathepsin-C gene located on the 11q14-q21 region of the chromosome, encoding a lysosomal protease in the interval between D11S4082 and D11S931. Thus, impaired function of cathepsin C gene in epithelial regions lead to abnormalities like thickening of the palms and soles.4, 5, 6, 7, 8, 9, 10, 11, 12, 3, 13, 14, 15 Thus, mutation in lysosomal protease enzyme which otherwise plays a pivotal role in maintaining balance between oral microflora and immune system by protein degradation and activation of proenzyme, leads to altered host response and hence failure of bacterial clearance from the gingiva causing destructive periodontitis resulting in tooth loss.2, 4, 5, 6, 7, 8
The onset of symptoms is between 1 and 4 years of age. In our all three cases, the symptoms were started between 2-3 years.10 The typical clinical features of PLS include palmar‑plantar hyperkeratosis and generalized aggressive periodontitis accompanied by severe alveolar bone destruction, leading to early loss of both primary and permanent dentitions. In our cases there was early exfoliation of all deciduous teeth within 2-3 years after eruption. The clinical manifestations observed in our patients were hyperkeratosis of the palms, and soles. The lesions were diffuse, with a dry, scaly surface; they varied in thickness and were rough on palpations and with generalized aggressive periodontitis, similar to all other studies.9, 10, 11, 12, 3, 13, 14 Hairs and nails appeared normal in all cases. Seasonal variation of skin lesions in papillon-lefevere syndrome are not well documented. The positive history of manifestation of recurrent pyogenic skin infections since childhood was documented by Subramanium et al. In our case the palmoplantar keratosis was not aggravated by seasonal changes.5, 6, 7, 8, 9
In PLS generally, vertical alveolar bone loss is seen around the incisors and first molars. The vertical pocket formation, with bone loss often more extensive which differ from horizontal type of bone loss in chronic periodontitis. OPG of all patients showed extensive alveolar bone loss upto apical one third of all remaining permanent teeth giving floating-in-tooth appearance.1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 3 Clinical findings like liver abscesses and radiological findings like intracranial calcification had been reported by Almunnef et al., were absent in current cases.8, 9
In patients with PLS, routine blood investigations and liver function tests usually yield values within normative ranges. According to Almuneef et al., Neutrophil counts, lymphocytes counts, and/or monocytic function are decreased in some patients.15 But in our case Hb and MVC value decreased while differential counts and ESR is increased.
Hiam-Munk syndrome is similar to PLS with respect to prepubertal periodontitis and palmo-plantar hyperkeratosis, but sufferers also exhibit arachnodactly, acroosteolysis and deformity of the phalanges of the hand.1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 3, 13, 14 Palmoplantar ectodermal dysplasia (PPED) is a skin condition that include 8 types, PPED type 4 which resembles the PLS in skin manifestations but PPED also exhibits disturbances in other ectodermal derivative and it does not cause aggressive periodontitis.1 Another consideration is Acrodynia, also known as Feer’s syndrome which usually caused by mercury intoxication. It characterized by dusky pink discoloration in hands and feet and loss of teeth. But, in addition, there is erythocyanosis, muscle pain, insomnia, sweating, tachycardia and psychic disturbances. Acrodynia is seen in children between the ages of 6 months and 4 years but it does not cause palmoplantar keratosis.1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 3, 13 Another condition of interest in differential diagnosis is hypophosphatasia. In addition to the clinical features of knock-knee, bowing of femur and tibia and enlarged wrists, the teeth are prematurely shed and are hypoplastic. Diagnosis can be made on the basis of increased amounts of phosphoethanolamine in the urine.1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 3, 13, 14
Treatment modalities for papillon-lefevere syndrome requires a multidisciplinary approach. The dental treatment comprised involved a professional prophylaxis, scaling and root planning, basic instructions on oral hygiene and use of 0.12% chlorhexidine mouth rinse. Further treatment should involve pedodontist for extraction of hopeless teeth which have severe bone loss with replacement of edentulous arches with prosthesis. Dermatological manifestations are usually treated with emollients, and salicylic acid and topical steroids may be added to enhance their effect.
Conclusion
As all the three case showed characteristics features of PLS syndrome, it is important for dental professionals to have a thorough knowledge to identify the disease in its very early stages. Dentist is usually the first member of health team to see this interesting and challenging diagnostic problem. Early diagnosis with proper treatment plan not only prevent or delay tooth loss, but also decreases risk of social, psychological and economical stigma. In our case patient’s parents were consanguineous married and unaware of disease as they came to hospital when all siblings showed dental problem, which also increases genetic risk to their offspring. It is very important to give awareness of syndrome and to provide appropriate and comprehensive dental care including establishment of functional rehabilitation.


