Introduction
Early childhood caries is one of the most prevalent chronic childhood diseases worldwide. More than 532 million children worldwide are affected by dental caries of primary teeth, and it is frequently observed in unprivileged groups in developing countries.1, 2 Although, dental caries is a preventable and controllable oral disease, still a great burden had to been put on curative care. The prevalence of untreated cases of dental caries in young children remains a deep-rooted challenge. It may be because standard dental therapies for caries are either beyond reach or unaffordable to most of the pediatric population.2
Even though, fluoride application is considered as a well-established primary preventive measure, several children present with deep carious lesions which involve deeper part of the dentine. These teeth need removal of carious tissues using rotary instruments or manual excavation followed by restoration which results unpleasant dental experience in pediatric patients. Extensive tissue loss may lead to dislodgement of restorations, repeated infection, and indirect restorations. Apart from that, management of uncooperative pediatric patients may demand lengthy treatment sessions or advanced forms of behavior management such as sedation or general anesthesia. These are essentially posed burden to dental units, especially in developing countries.3
The Covid-19 is a highly contagious viral disease which has become a huge burden globally since 2019. It is a disease caused by the pathogen, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).4 On January 31, 2020, the World Health Organization (WHO) announced that the Covid-19 outbreak had become a public health emergency of international concern. Later, it was categorized as a pandemic on March 11, 2020.5
According to the scientific evidence, interpersonal transmission is possible via infected respiratory droplets by direct or indirect contact with nasal, conjunctival, or oral mucosa, when respiratory particles are inhaled or deposited on these mucous membranes.6 Emerging evidence of the airborne risk of Covid- 19 virus should also be taken into consideration.7
The Covid-19 pandemic has shaken the global healthcare structure and oral healthcare has been no exception. The World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC) guidance on oral health services, and the Cochrane community recommended delaying routine dental care. Around 60.8%, 35.5% and 18.3% of preschool aged children in Wuhan, China had self-reported dental cavities, toothache, and halitosis, respectively.8 Most of the people who suffered with dental problems did not visit dental clinics due to limited dental services during the pandemic and fear of contracting the Covid-19 virus through dental care.9
Alternative measures had been discussed in the literature to offer dental assistance during these unusual times, such as teledentistry, online visits and over the phone advice.10, 11 Non / low aerosol generating procedures are good alternatives for caries management in midst of Covid 19. Use of SDF is an efficacious and safe approach especially for pediatric patients in both pandemic and post pandemic period.
Efficacy of SDF in dental caries prevention and arrest
Silver diamine fluoride (SDF) is a clear liquid containing silver, fluoride and ammonia complex that has been identified as a promising therapeutic agent against dental caries in both primary and permanent dentition.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 It combines the antibacterial effects of silver and the remineralizing effects of fluoride, which makes the SDF a good treatment option for managing caries lesions.12 In-vitro studies showed significantly less number of S. mutans and L. acidophilus within the lesions treated by local application of SDF, supporting the fact that SDF possessed an anti-microbial activity against cariogenic bacteria.14, 15
Figure 4
Clinical appearance: After 2 weeks of SDF application (no signs of infection or inflammation)

Further, studies demonstrated the ability of SDF to slow down the demineralization process of dentine by preventing collagen degradation by inhibiting Matrix metalloproteinases and cathepsins.15, 16, 17 Many clinicians working on caries prevention therapies have presented steady findings and emphasized that SDF is surely more potent than the fluoride varnishes in arresting dental lesions with no reported evidence of pulpal damage post application.2
Most of the clinical studies in literature used 38% of SDF solution and it is the recommended strength of SDF to be used to achieve better results.13, 14, 15, 16, 17, 18 The clinical effectiveness of 38% SDF solution in arresting dental caries of primary teeth and preventing and arresting root caries in adults has been consistently supported by all of the systematic reviews.19, 20, 21 As stated by Gao et al. in 2016, the overall proportion of arrested dental caries following SDF treatment was 81% (95% CI, 68% to 89%; P < 0.001).20 SDF application on carious primary teeth shows promising results in arresting and preventing of caries when compared with use of fluoride varnish. A prospected controlled clinical trial carried out by chu et al. in 2002, showed that an annual application of 38% SDF was more effective than 3 month application of 5% NaF varnish in arresting dentinal caries of primary teeth. Results of this study agree with observations of many other studies.22, 23, 24
A randomized controlled study by dos Santos Jr VE et al. compared the efficacy of 30% SDF with of Glass Ionomer Cement (GIC) when used as an intermediate restorative technique (IRT) and found that SDF was 1.73 times more effective in arresting caries than IRT.25
Contraindications and considerations for SDF use
SDF had been used for over 80 years with no serious complications.18 However, use of SDF is contraindicated in patients with silver allergy, clinical/ radiographic signs, or symptoms of periapical pathology and significant desquamative gingivitis or stomatitis.26, 27 Black discoloration of the lesions, staining every surface it contacts and temporary metallic taste are the commonly claimed side effects of SDF application. Even though some studies supported use of Potassium Iodide (KI) with SDF to reduce the discoloration, insufficient evidence exists to conclude positive clinical results.28 Despite the advantages, use of SDF will be less popular in dental practice due to compromised esthetic. However, literature reports poorer parental acceptance for use of SDF in anterior teeth compared to posterior teeth.29, 30, 31, 32 Sultan A et al. (2020) reported that parental acceptance was significantly less for teeth located in esthetic zones such as maxillary incisors and in children below three years of age.29 But the willingness of parents for SDF was increased with the level of uncooperativeness of the child.29, 30, 31, 32, 33 An umbrella review done by Sabbhag et al. on 2020, stated that pre-operative instructions could significantly improve parental acceptance of SDF application.32 The average lethal dose of SDF by oral and subcutaneous administration was 520 mg/kg and 380 mg/kg, respectively. One drop of 38% SDF liquid contains 9.5 mg silver diamine fluoride. One drop of material is sufficient to treat up to five teeth.34 The recommended dosage is one drop (25 μL) of 38% SDF liquid per 10 kg of body weight child per treatment visit.34
Clinical Technique
Preparation
Cover the work-surfaces with plastic wraps to avoid stains due to SDF and use plastic bibs for the patient.
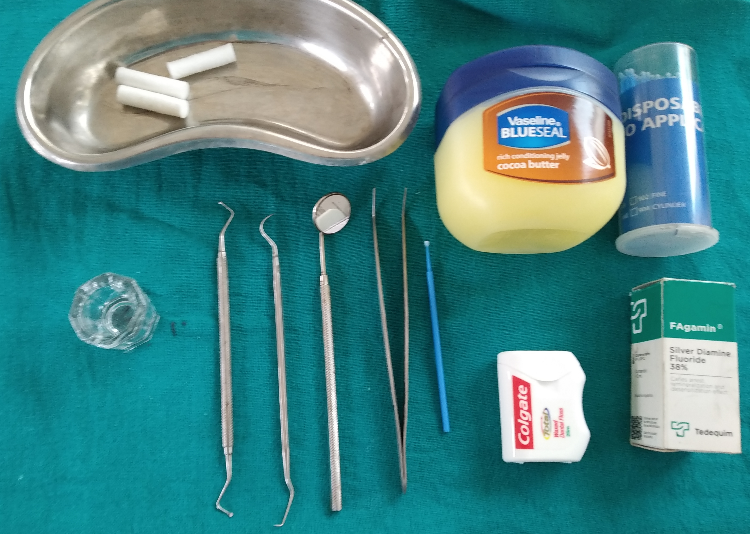
Take precautions to minimize unwanted side effects. Use maximum isolation with rubber dam or if is not possible due to poor cooperation, cotton wool rolls and gauze can be utilized. Application of petroleum gel around the lips and vermillion borders will reduce the risk of staining. [Figure 1]
Caries removal
Removal of carious tissue is not indicated prior to application of SDF as it does not show added advantage in caries arrest.37 However, removal of gross debris from cavities will allow better SDF contact with denatured dentin and removal of infected dentine will sufficiently reduce the bacterial load.18
Application of SDF
SDF solution (38%) should be applied directly over the dried carious lesions using a micro brush. Minimum but adequate amount of the solution is used cautiously to prevent inadvertent gingival discoloration. No more than one drop of 38% SDF solution is recommended in one visit. [Figure 2] [Figure 3] It is ideally recommended to remove the excess SDF using cotton pellets/ gauze, after leaving one to three minutes in contact.34
Follow-up
Follow up visit is recommended after 2-4 weeks of the first application of SDF to check the efficacy of the procedure done. [Figure 4] If the lesions do not show features of an arrested site (Dark brown color, hard texture), reapplication is indicated.38
Restorations after SDF therapy?
SDF therapy is proven to arrest dentin caries and it results a black deposit on the treated site which may cause an esthetic concern of both parents and the child. A tooth-colored restoration can mask the stains caused by SDF- arrested dentine caries and recontour the tooth into functional shape. Placement of GIC restoration on SDF treated, arrested lesions, following the concept of ART improved parental satisfaction significantly.39 Previous application of SDF does not show an influence on bonding strength between GIC and the dentine.40 SDF is a valuable option of non-surgical caries management in is COVID-19 era.
Dental clinics carry a high risk of cross infection due to the nature of dental treatment and it is critical for the Covid-19 because of the aerosol generating dental treatment procedures. So, routine dental treatments and elective procedures were suspended across the world during this period. This in turn has caused an upturn in the numbers of children suffering from dental caries. Dental professionals around the world are confronting the consequences of disrupted oral health care during the pandemic. There are many reasons for this including lack of access to care, or a personal decision to forgo care due to fear of contracting the infection in the dental office, or lack of focus on home oral care due to altered diet patterns, sleeping patterns and limited affordability or availability of oral hygiene products during the pandemic. Since caries removal is not necessary during treatment with SDF, it accounts under non-aerosol generating dental procedure. Yet, it gives good clinical results in caries arrest and prevention. Application of SDF is a simple procedure that keeps the treatment session short, even with less cooperative pediatric patients.24, 25, 26 Furthermore, guidelines and recommendations on Covid-19 global pandemic induced dental practice modifications pertaining to pediatric dentistry highlighted the importance of using SDF underpinned minimally invasive dental practice to mitigate infection transmission by aerosol generation.
Conclusion
Use of SDF is a better principal that can be practiced enhancing prevention and minimal operative intervention. More importantly, it is a child friendly, cost effective and successful management strategy. SDF application could be carried out with minimum facilities. Therefore, promoting the use of SDF is an effective treatment mode particularly during a pandemic such as Covid-19.