Introduction
From past few decades, the replacement for the missing teeth is done by the dental implants that are also called as oral or endosseous implants. Due to their high success rate and high predictability, these are revolutionary as well as extremely important additions to the dentistry. Implants assimilate to the surrounding tissues, upon which, their success rate depends. Assimilation of dental implants depends upon numerous factors like quantity and quality of bone, material of the implant as well as the loading condition. Neighbouring soft and hard tissues around the implants are known as peri-implant tissues. There should be an intimate relationship among the surface of the implant and the surrounding bone and this relationship is called as osseointegration.1
For now, the most widely used implants are the osseointegrated implants. The main shortcoming of these implants is that these lack the periodontal ligaments as present in the natural dentition. The osseointegrated implants are ankylosed and lack physiological mobility as the natural teeth and also lack the shock absorbing capacity as compared to the natural teeth. Periodontal ligaments consists of various types of cells like fibroblasts, osteoblasts, cementoblasts, cementoclasts, osteoclasts and undifferentiated mesenchymal stem cells responsible for the productive relationship among the bone and the tooth.2
Periodontal ligaments, present in between the alveolar bone and cementum of the teeth, have a crucial role in the regulation of the bone as well as tooth support in the alveolus. Different types of progenitor cells are seen in these tissues, crucial for maintaining the homeostasis of the periodontium. Lately, periodontal ligament stem cells are used for therapies related to the titanium dental implants such as implants coated with these cells and hence can be considered as substitutes to the osteointegrated implants.3
In the past few years, LIGAPLANT, that is a combination of the implant biomaterial along with the Periodontal ligament cells has become a new strategy for the replacement of the missing tooth and it provides a better biological performance as it includes the development of the periodontal ligament attachment surrounding the dental implants.4
Rationale
As ligaplant is an amalgamation of the periodontal ligament cells and implant biomaterial, thus periodontal ligaments formed facilitates the micro movements and shock absorption contrary to the conventional implants and have a positive impact on the quality of the distribution of forces among the teeth abutments and prosthesis supported by the implants. Their use may overcome the shortcoming of the conventional implants and may provide better physiological results that can lead to increased lifeline of the prosthesis as these implants mimic the form and function similar to that of natural teeth.
PDL Integration versus Osseointegration
The conventional osseointegrated implants lacks the fibrous capsule and also the interfacial layer at the interface of the titanium and bone have abundant noncollagenous proteins and few plasma proteins. The implant-bone interface of these implants is rigid due to which these do not possess crucial properties such as biological remodelling and plasticity leading to the lack of the mobility while the functional loading. This results in the shift of extreme stresses to the adjacent bone responsible for the loss of the marginal bone. Whereas, incorporation of the periodontal ligaments around the dental implants may help in the cementum formation on the surface of the implant along with the periodontal attachment apparatus comprising periodontal ligament fibers and the sharpey’s fibers supporting the remodelling of the bone.4
Characteristics of Ligaplants
Induces proprioception i.e. the sense of the self-movement and position of the body.
It helps in the distribution of the occlusal as well as masticatory forces.
Provides shock absorbing capacity opposite to the conventional implantst.
Due to the presence of undifferentiated cells of different types, these also provide osteoconductive properties to the implant.y
Provides anchoring similar to natural dentition, facilitating tooth movements while the orthodontic therapy.
Provide suitable anchoring for development and growth of alveolar bone housing.5
The Basic Concept in Foundation of the Ligaplant
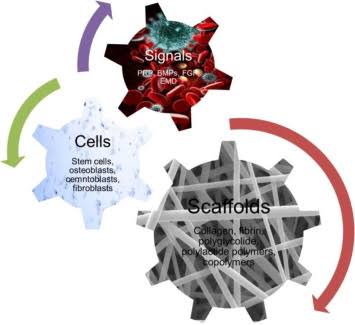
Tissue engineering has become a revolutionary strategy for the preparation of the scaffolds made up of biodegradable polymers with growth factors that can facilitate production of the tissues. It is based on the principle of life sciences and engineering. Osteoconductive matrix along with the tissue engineering products upgrades advantageous effects of these materials by revascularization and increasing cellular ingrowth. To the original cementum of the teeth, a layer of cementum gets attached with which the regeneration starts and into which freshly formed transverse fibers gets consolidated.6
By merging the three main principle constituents, the concept of the tissue engineering is interpreted as a triangle that states that combining these elements will facilitate regeneration. These key elements are scaffolds or matrix, signalling molecules and cells. Scaffold used, will act as a three-dimensional structure and will facilitate the migration and proliferation of the cells and leads to the formation of matrix leading to the development of the tissue.7
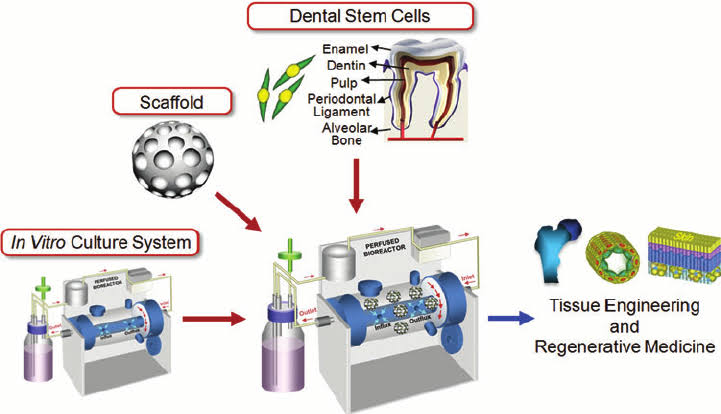
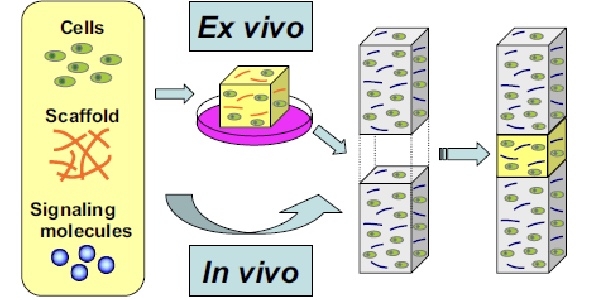
By using the signalling molecules, over the biodegradable matrix and scaffolds, the cells are cultured, after which these are transplanted to the body. This technique is called as the in vitro technique. On the other hand, the cultivated vital elements are deposited in the tissue defects followed by the physiological process of the healing in body leading to the regeneration. This technique is called the in vivo technique that causes the intrinsic healing activity by the use of these three elements of tissue defect sites. Ligaplants can be procured by both in vivo and in vitro technique.9
Figure 3
Ex vivo technique- For the formation of the organs and the tissues in a culture room by amalgamation of the scaffold or matrix, cells and signalling molecules prior to the transplantation of newly tissue-engineered organ to the patient’s body. In vivo technique facilitates intrinsic healing activity at the required site.10
Procedure of Obtaining Ligaplants
After the extraction of the donor tooth, it is immediately replanted into its native alveolus 14 days prior to its transplantation. There is cell proliferation and differentiation due to the activation of the process of healing within the periodontal ligament, caused by the intentional trauma. Tooth can be transplanted after fourteen days, at the time, when the cell culture reaches its peak with various cells at the root surface attached by freshly formed sharpey’s fibers.
An identical cell culture, by utilizing tissue engineering around an artificial root is a new concept that has been introduced to produce ligaplant by the following three steps:
Step I- Preparation of temperature responsive culture dishes
N-isopropylaclamide monomer in the solution of 2-propanaol was expanded onto polystyrene culture dishes. By using an Area Beam electron processing system, irradiation of the electron beam was put through these dishes. For the removal of the ungrafted monomer, rinsing of these dishes is done and are sterilized with ethylene oxide.
Step II- Cells and the cell culture
Human periodontal ligament cells are then taken by scraping the middle third of the root periodontal tissues from an extracted tooth, by using a scalpel blade. Then these tissues are planted into the culture dishes having Dulbecco’s modified Eagle’s minimal essential medium augmented with 100 units/ml of penicillin-streptomycin and 10% serum of fetal bovine. These out growth cell are then cultured by providing a humidified atmosphere of 5% carbondioxide at a temperature of 37 degrees for 48 hours to facilitate the attachment of cells to the dishes. The medium needs to be changed at least three times in a week and the debris are removed by washing these dishes. At 37oC along with ascorbic acid 2-phosphate (50mg/mL), 10nM glycerophosphate and 10nM dexamethasone and a cell density of 1x 10,5 the human periodontal ligament cells are kept on a temperature- responsive culture dishes that are 35mm in diameter. It acts as a medium for osseodifferentiation for procuring the cell sheets.4
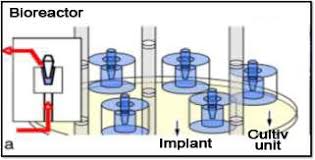
Step III- Culturing of the cells of periodontal ligament in a bioreactor
Titanium pin that is glazed with hydroxyapatite is kept in a hollow cylinder made up of plastic and also around 3mm of gap is kept around the pin. By this 3mm gap, the culture medium is constantly pushed. For around 18 days, single cells suspension procured from humans is implanted into the vessels made up of plastic under the flow of growth medium.11
Precautions while Preparing the Ligaplants
There should be small mechanical movements of the medium flow while the preparation of the ligaplants. There should be optimal space in between the implant and the culture. Time for which the surface treatment is done should also be optimal for the procurement of a good Ligaplant. Adequate sterilization is also necessary. The culturing of the cells should be optimal to prevent the growth of non-periodontal ligament cells.10
Advantages
These implants can be planted in areas where conventional implants cannot be placed that are in areas of the bony defects.
Identical to the natural insertion of natural tooth roots in the alveolus
These get firmly co-ordinated with no bone contacts and with no interlocking, inspite of the existing loose fitting for sparing the periodontal ligament cushion of the cells.
Induces formation of the bone and also an intimate tissue communication along the surface of the implants and bone is seen.
Disadvantages
The procurement of ligaplants is a technique sensitive process and its success depends on the optimal temperature, cells utilized for the culturing purpose, time for which the culturing is done and many more.
Other non-periodontal cells can grow instead of the desired one in case of any complications in the process of culturing.
High cost is another important drawback of the ligaplant as there are limited facilities and labour
Implant failure can also occur because of the incalculable factors that may affect the acceptance of the implant by the host and also the growth of the periodontal ligaments. 12
Risk Factors of Ligaplants
The process of developing periodontal ligament in order to produce the periodontal ligaments entirely depends upon the site signalling that is mainly mediated by homeogene-coded transcription factors and by anatomic code. These homeoproteins are important for the formation of the signalling components as well as the cell surface. Factors that influence the growth of the periodontal ligaments at the required site are usually uncertain and hence act as risk factors for the treatment outcomes.
Success of Ligaplant
To produce a regenerative periodontal ligament, site-specific signalling is a crucial factor that is consecutively mediated by an anatomic code that is written in expression patterns of Homeogene-coded transcription factors. Therefore, synthesis of the surface of the cells and signalling components is affected by the homeoproteins, the signals from the surface of the cell react to modulate Homeogene expression that leads to the establishment of the cell identities as asporin that is an SLRP protein existing in extracellular matrix has been discovered.13
Ethical Applications
Ligaplants, a revolutionary new strategy, has been clinically tested in vitro as well as in vivo. Various studies on animals have reported positive results but correlation of results of the in vivo studies are still to be done. As per the strong evidence reported in the literature, this can be the near future of the implant therapy as it can provide the function, form and responses identical to that of the natural teeth.9
Evidence Based Studies
As per the study conducted by the Nyman S et al in the year 1982, the cells present in the periodontal ligaments have the capability to re-establish attachment of the connective tissue to the teeth surface.14 Nunez et al in the year 2012 confirmed the regenerative capacity of the periodontal ligament derived cells.6 Lin et al in the year 2011 used rat periodontal ligament cells for the purpose of regeneration of the periodontal tissue on the titanium implants. A 3-dimensional scaffold was used that contained abundant extracellular matrix for the regeneration of the periodontal ligaments at the interface alveolar bone-titanium-implant. High levels of proliferation rates, clonogenicity and tissues identical to cementum were noted on the Titanium implant surface. Also sharpey’s fibers were inserted perpendicular to the implant site.15 Rinaldi et al in year 2010 evaluated the placement of the titanium miniplants in twenty-four rats between the buccal roots of the mandibular first molar. After 21, 30, 45, 60, 90 and 120 days after the plantation ultrastructural analysis was done.15 Byung-Ho Choi in the year 2000 used Ti screw-type implant with periodontal ligaments cells used from the mid surface of root. Results of this study showed that there was formation of the periodontal ligament type tissue in between the alveolar bone and cementum like tissue.16 Buser et al in the year 1990 evaluated the development of the cementum on the implants that are sprayed with plasma, transplanted to the alveolus, after about 12 months. They reported the development of a hard layer of tissues on the surface of the implants that have continuity with the freshly formed cementum that have its source from the cells of periodontal ligaments from the adjoining tooth.17
Conclusion
The implant dentistry has been transformed by the Introduction of periodontal tissue engineering. Based on the modality, ligaplants have been recently introduced to overcome the shortcomings of the conventional implants. Majority of the studies related to the ligaplants, done on the animals has shown successful results but still more achievable and practical way of procuring the periodontal ligament attached implants needs to be introduced. Also more human studies need to be done to evaluate the successful outcome of this strategy. As ligaplants has various advantages in comparison to conventional implants, these can emerge as a new revolutionary addition to the implant dentistry.4