- Visibility 116 Views
- Downloads 7 Downloads
- DOI 10.18231/j.ijohd.2020.048
-
CrossMark
- Citation
Flapless soft tissue punch technique for implant placement- A case report
- Author Details:
-
Dhwani K Dedhia
-
Vijayalakshmi Rajaram *
-
Jaideep Mahendra
-
Devi Parameswari
-
Satheesh Khanna
Introduction
Dental implants are defined as biologic or alloplastic biomaterials surgically inserted into hard or soft tissues of the mouth for functional or cosmetic purposes.[1] Since 1970s, modern Implantology is based on the concept of surgery with flap elevation. The first incision followed the protocol designed by Brånemark which was performed in the oral vestibule; so when flap was replaced, the incision line and suture remained separated from the location of the implant, thus trying to prevent infection in the surgical area.[2] Gradually, several clinical trials demonstrated that a midcrestal incision gave similar success rates compared to those obtained using the classical protocol. In addition, midcrestal incision produced less swelling and inflammation.[3]
The success of oral implant treatment depends on the synergy between patient factors, treatment planning, surgical technique, prosthodontic and technical aspects of the implant restoration.
More recently, the concept of flapless implant surgery has been developed for patients with sufficient keratinized gingival tissue and bone volume in the implant recipient site. In a flapless procedure, a dental implant is installed through the mucosal tissues without reflecting the flap. Two types of flapless implant surgery are mainly the direct drill technique and the soft tissue punch technique.
Case Presentation
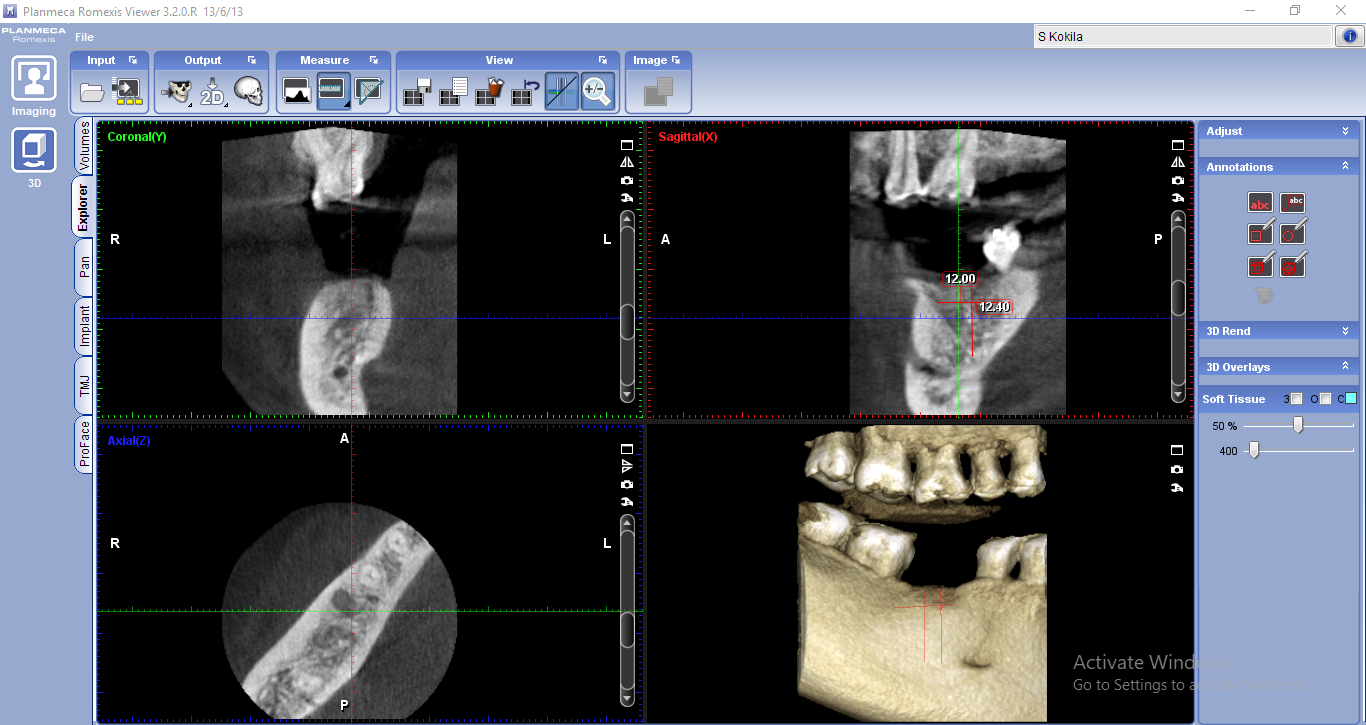
A 42-year old systemically healthy female patient reported to the Department of Periodontology with the chief complaint of edentulous space in lower right back tooth region for the past 1 year. The clinical examination showed edentulous space in relation to 46 with no mesial drifting of 47 or supra-eruption of 16 ([Figure 1]). Radiographic examination revealed adequate bone height and bone width. CBCT in relation to 46 was taken and bone mapping was done to assess the accurate bone height and bone width ([Figure 2]). The treatment plan included phase I therapy followed by implant placement in relation to 46 after 1 week. The treatment plan was explained to the patient and written informed consent was obtained for the same.

Case Management
Phase I therapy
Phase I therapy was done in the first visit.
Surgical therapy
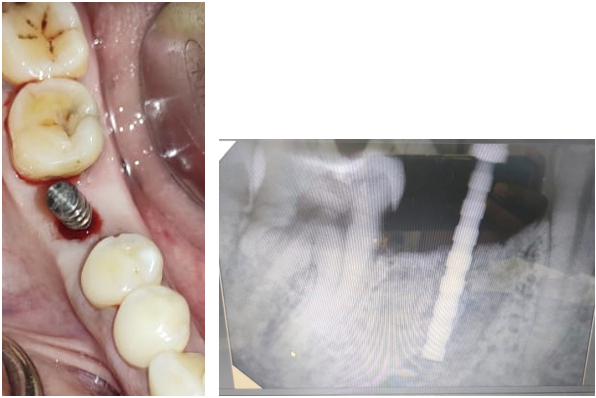
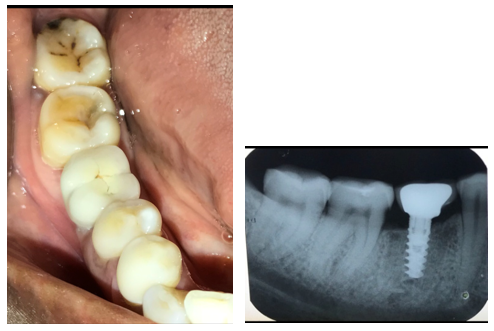
Preprocedural mouthrinse of 0.2% chlorohexidine was administered before the start of the procedure. After infiltration of local anaesthesia (2% lidocaine) in relation to 46, a soft tissue punch of diameter 4mm was used to punch out the soft tissue at the surgical site ([Figure 3]). The osteotomy site was prepared using an initial round bur and a 2mm twist drill with copious amount of saline irrigation and parallelism was checked ([Figure 4], [Figure 5]). This was followed by subsequent drills of different height and diameters to achieve the desired height and width. Adin implant of size 4.2*10mm was placed in the osteotomy site (Fig 6) and a healing cap was placed on the implant. Immediate post-operative radiographs were taken ([Figure 7]). Post-operative instructions were given to the patient. Medications included Amoxicillin 500mg thrice daily for 3 days and Zerodol-P twice daily for 3 days. The patient was reviewed at 1 week, 2 weeks, 4 weeks and 4 months. No severe pain or discomfort was reported by the patient. Healing was uneventful. The final prosthesis was given after 4 months ([Figure 8]).




Discussion
Minimally invasive surgery is the current trend which aims to perform surgical procedures infringing as less damage as possible to the patient through minimal incisions by reducing the size of the instruments.
Albrektsson et al. in 1986 proposed certain criteria to assess success of implants. According to these criteria, bone loss of less than 0.2 mm annually following the implant’s first year of function is stated as being essential for long-term success.[4] Since then, the crestal bone area has been considered as a significant indicator of implant health. Establishing intact papillae and gingival contour around implants is of utmost importance, especially in patients who display soft tissue during function, such as speaking and smiling. Salama et al.have established that the interproximal height of bone is an important factor in achieving optimal esthetic outcomes.[5]
Anumala et al[6] compared the soft tissue profile and height of crestal bone levels using radiovisiography around single-stage implants after single-piece implant placement with two different surgical techniques, that is, open flap procedure and flapless (FL) procedure in thirty patients. The results concluded that the flapless implant surgery resulted in lesser loss of interproximal bone and also resulted in better soft tissue changes (reduction in the papillary bleeding index, reduction in the sulcus bleeding index and reduction in the mean probing pocket depth) when compared with the open flap technique.
The disadvantage of flapless implant surgery is that it is a “Blind technique” i.e; the surgeon’s inability to visualize anatomic landmarks and vital structures due to lack of flap reflection. This can be resolved with the help of CBCT and bone mapping.
The advantages of flapless implant surgery are that it is atraumatic, reduced surgical time, lower patient morbidity, increased patient comfort, high survival rate along with the preservation of the keratinized soft and hard tissue volume at the surgical site, preservation of circulation, and accelerated recuperation allowing the patient to resume normal oral hygiene procedures immediately after implant placement. Hence this flapless approach of implant placement is a new and efficient technique for implant placement with less time consumption and lower patient morbidity.
Conclusion
Recent advances in implant therapy have made implant placements more efficient. Minimally invasive approach of implant placement has proved to be more efficient than the conventional method and has a high patient compliance. This case report uses flapless soft tissue punch technique for implant placement.
Source of Funding
None.
Conflict of Interest
None.
References
- Z Sheikh, N Hamdan, Y Ikeda, M Grynpas, B Ganss, M Glogauer. Natural graft tissues and synthetic biomaterials for periodontal and alveolar bone reconstructive applications: a review. Biomater Res 2017. [Google Scholar]
- M M Romero-Ruiz, R Mosquera-Perez, J L Gutierrez-Perez, D Torres-Lagares. Flapless implant surgery: A review of the literature and 3 case reports. J Clin Exp Dent 2015. [Google Scholar]
- S Kumar, R Aggarwal, S Jain, S Choudhary, T Kaur, N K Reddy. A Radiographic Evaluation of Peri-implant Bone Level in Immediate and Conventionally Loaded Implants Using Flap and Flapless Techniques. J Contemp Dent Pract 2019. [Google Scholar]
- W Geraets, L Zhang, Y Liu, D Wismeijer. Annual bone loss and success rates of dental implants based on radiographic measurements. Dentomaxillofac Radiol 2014. [Google Scholar]
- H Salama, M A Salama, D Garber, P Adar. The Interproximal Height of Bone: A Guidepost to Predictable Aesthetic Strategies and Soft-tissue Contours in Anterior Tooth Replacement. Craniofac Growth Ser 2001. [Google Scholar]
- D Anumala, M Haritha, S Sailaja, E Prasuna, G Sravanthi, N R Reddy. Effect of Flap and Flapless Implant Surgical Techniques on Soft and Hard Tissue Profile in Single-Stage Dental Implants. J Orofac Scie 2019. [Google Scholar]
