Introduction
The functions of maxillary and mandibular teeth are monitored primarily by the periodontal ligament (PDL) which harbours a rich innervation, carrying refined mechanoreceptive properties by an intimate contact between collagen fibres and Ruffini-like endings1 [Figure 1]. Normally the afferent sensory impulses relay its information to the central nervous system, which successively results an efferent response and the initiation of muscle activity is produced. After extraction of teeth, this feedback pathway could be damaged and ends in loss of function, impaired aesthetics, and loss of the PDL and its mechanoreceptors.2
Edentulism or patients with partial edentulism are treated with the choice of removable prosthesis which is inherently unstable during jaw movements and this ends up in difficult in mastication, painful to the underlying structures and diet and nutrition suffer. Implants, the present treatment option for treating edentulism or partial edentulism provide alternative treatment options for such patients to provide better functional integration which induces a certain tactile sensitivity property called as “osseoperception”.3
Online research using various free search engines like Pubmed and Google scholar has been carried to produce scientific evidence of osseoperception to retrieve studies published between 1985 to 2019 using the subsequent keywords: “osseoperception’’, “mechanoreceptors”, “tactile sensibility”. This article reviews the literature and throws light on certain aspects of osseoperception.
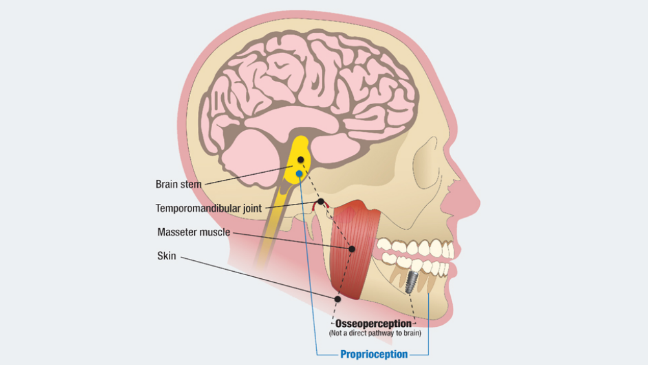
Osseoperception is defined as mechanoreception in the absence of a functional periodontal mechanoreceptive input and it is derived from TMJ, muscle, cutaneous, mucosal, periosteal mechanoreceptors which provide mechanosensory information for oral kinaesthetic sensibility in relation to the jaw function and the contacts of artificial teeth.4 [Figure 2].
Neurophysiological mechanisms that modulate jaw movement are related to the sensory structures that are present in and around the Osseo integrated dental implants.5 To control oral motor functions like chewing, biting, speech etc., the central nervous system (CNS) relies information from the sensory organs within the orofacial structures. Teeth are equipped with tactile sensors like periodontal mechanoreceptors that provide feedback of magnitude, direction, and rate of occlusal load application for sensory perception and motor function. Periodontal nerves react to touch, pressure sensation and tooth position as well as to tissue injury. Ruffini endings are the specialized nerve terminals, which are low threshold stretch mechanoreceptor are the primary periodontal mechanoreceptors present in the periodontal ligament which are responsible for touch, pressure sensation.6
Figure 1
The natural tooth contains a periodontal ligament, whereas an implant lacks a PDL and has a direct bone interface
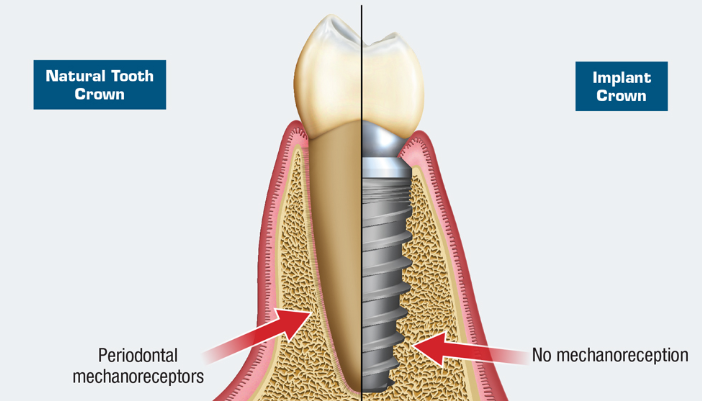
The periodontal mechanoreceptors (PDMs) have a key role in sensory discriminative capabilities and provide feedback on the magnitude, direction and rate of occlusal load for sensory perception and motor function of the jaws (proprioception). Although an implant lacks this protective mechanism against biomechanical force overload, it does receive minimal mechanoreception from the temporomandibular joint, associated musculature and cutaneous structures (osseoperception).
Discussion
Physiological integration of osseointegrated implants indicates the presence of peri-implant innervations influencing the oral function. Regeneration of nerve fibres are seen at the bone remodelling and growth interface after implant placement.
Linden and Scott in 19897 succeeded in vitalizing the nerves of periodontal origin in healed sockets, which suggests that some nerve endings remain functional. These experiments resulted in the talk on the existence and potential function of sensory nerves fibres within the bone -implant environment. Histological evidence showed the appearance of some reinnervation around implants.
Placement of implants may cause degeneration of environing neural fibres by surgical trauma. However, wado et al in 2001, observed the development of new fibre and also increases in the number of free nerve endings near the bone-implant interface during the primary weeks of healing.8
A study by Jahangiri at al (2005)9 on the dog has succeeded in partially regenerating the periodontal ligament on an implant surface. Whether such regeneration may additionally induce restoration of the peripheral feedback pathway has however not been studied.
Jacobs et al 200610 Sensory nerve fibres are damaged at large numbers after tooth extraction. After extraction, the myelinated nerve fibre content of the inferior alveolar nerve is reduced by 20%. These fibres which were originally innervating the tooth and periodontal ligament are still present within the inferior alveolar nerve.
Livia dos Santos Corpas et al., in 2014 explained about peri-implant nerve fibres that are present around osseointegrated implants in humans.11 Presence of both myelinated and unmyelinated nerve fibres are recognized inside the Haversian canals of bone near the implant threads. Myelinated fibres were also spotted at the woven bone around the implant. However, no differentiated nerve endings could be observed around the implants.
Existing mechanoreceptors within the periosteum also play a major role in tactile function on implant stimulation. Forces applied to osseointegrated implants are directly transferred to the bone which in turn produce bone deformation leading to receptor activation in the bone implant region.12
Methods to evaluate osseoperception
Oral perception sensibility of dental implants can be checked by applying pressure either on the occlusal surface of the implant passively as described by Enkling et al (2012). They can be checked by passive tactile sensibility, or active tactile sensibility. Passive tactile sensibility study involves testing only the individual neural receptors, whereas, active tactile sensibility more effectively represents normal function.13
Enkling N et al., in 201014 compared the passive tactile sensibility of natural teeth versus osseointegrated dental implants within the maxilla. They concluded that osseointegrated implants subjectively feel “touch” sensation when greater force is applied when compared with the tactile function of natural teeth.
Lundqvist and Haraldson found active threshold is two to three times higher for implants and for implants the active threshold is about 50 times higher than that of natural teeth. Large discrepancy is due to several receptors group may respond to active testing, while the passive methods electively activate periodontal ligament receptors. The latter are eliminated after extraction, which explains the reduced tactile function in patients with no teeth.
Bone-implant prosthesis rehabilitation in patients with no teeth, seem to function quite well after rehablitation. These patients perceive mechanical stimuli exerted on osseointegrated implants. Improvement is seen in tactile sensibility with oral implants following a three-months healing period. This special sensory awareness with the bone-anchored prosthesis is osseoperception.
Judith et al., have shown that prostheses appeared to be well adapted to perform habitual masticatory functions in patients with implant-supported rehabilitation. The information revealed a less coordinated masticatory muscle activity during a nonhabitual function in the implant patients. 1
Concept of osseoperception helps us to retrieve the physiologic function with ossointegrated implant supported prostheses, despite the absence of periodontal mechanoreceptors which is considered the important component of neuromuscular coordination. However, an abnormal muscle reaction may be induced if eccentric function is not managed resulting in implant failures.
Increasing evidence of osseoperception in neurophysiology and histological studies demonstrated that this phenomenon may be attributed not only to neural endings in the bone–implant interface itself but also to neural endings located at some distance such as the periosteum, which was described as “osseoreceptors”.15
Neurophysiological evidence was obtained using functional MRI, showing an activation of the human sensory cortex after mechanical stimulation of incisor implants and teeth.16 The sensory nerve action potential of the inferior alveolar nerve stem could be recorded following stimulations to implants.
Conclusion
Root form implants are commonly used to restore teeth. To achieve satisfactory function with bone- implant prostheses, physiological and psychological integration of the implants should take place.
Presence of sensory perception is observed on patients with oral implants clinically on a later period of time. This mechanism of ‘osseoperception’ phenomenon still remains a matter of debate. However, further research is required to make practical use of osseoperception in the design of novel bone-anchored prosthetic appliances.