Introduction
Most injuries to the oral mucosa are painful and are a common reason for patients to choose self-treatment or to seek professional dental help. The etiological origins of such wounds are multiple; including mechanical injury, infection, inflammation etc. The clinical examination usually shows a slightly erythematous lesion with regular borders.1, 2, 3
Oral ulcers are a very common disorder of the oralmucosa. Mouth ulcers are common and are usually due to trauma suchas from ill fitting dentures, fractured teeth, or fillings, a bite (mainly at the cheek level), or a burn due to ingestion of food that is too hot.4, 5 Traumatic ulcer is usually a single lesion with erythematous, non everted margins and with a cleanbase covered with a pseudo membrane. Acute trauma in the form of a sharp puncture to the muscle is the main cause, but occasionally a history of trauma is absent, and the etiology is unknown.6, 7
Thermal and chemical burns causing ulcers
Chemical burn results from applying analgesics suchas aspirin or acetaminophen, to the mucosa adjacentto an aching tooth, mild white filmy desquamationseen in oral mucosa. Thermal burn is characterized by erosive lesion witherythematous borders surrounding whitish damaged mucosa. It usually involves palatal area and patient gives a positivehistory of eating or drinking something hot.8, 9, 10
Denture associated trauma
Lesions of the oral mucosa associated with wearingof removable dentures may represent acute or chronicreactions to microbial denture plaque, a reaction to constituents of the denture base material, or a mechanical denture injury. They include denture stomatitis, angular cheilitis, traumatic ulcers.11, 12
Apthous ulcers
Oral aphthous ulceration is another frequent cause of oral mucosal pain. Different types of oral aphthous ulcers exist: minor, major, or herpetiform. The most common is the minor aphthous ulcer, which affects 80% of patients presenting with aphthous ulcers. The lesion is round or oval, usually < 5 mm in diameter, with a gray white pseudomembrane and an erythematous halo.13, 14, 15
Whether caused by mucosal trauma or common aphthous ulceration, these benign lesions are a source of acute pain that can disturb daily activities (causing dysphagia, speaking impairment, etc).16
Hyaluronic acid
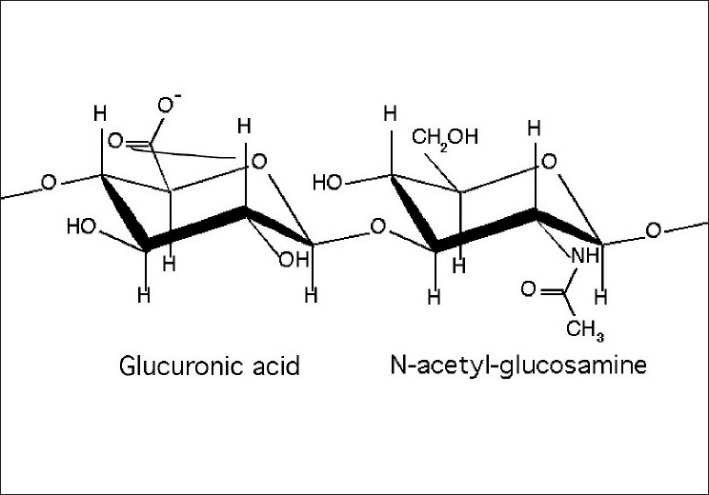
Hyaluronic acid (HA) is a linear polymer of glucuronic acid and N-acetyl glucosamine disaccharide. The main function of HA includes tissue healing including activation and moderation of the inflammatory responses, promotion of cell proliferation, migration, and angiogenesis. It also promotes re-epithelization via proliferation of basal keratinocytes. HA is a hygroscopic macromolecule and its solutions are highly osmotic. In the oral mucosa, this property enables to control of tissue hydration during periods of inflammatory process or response to tissue injury resulting in ulcer formation.17, 18, 19
Lignocaine
Lignocaine is a well-established and approved local anaesthetic alone and in combination used in a variety of topically applied preparations, mostly as medicinal product. It is also used to treat painful oral conditions in children, like aphthous ulcers, blisters, teething, or gingivitis.20
Lignocaine is an amide anesthetic that reversibly blocks the voltage-sensitive sodium channels in the membrane of a nerve cell. This blockage prevents impulses from being conducted along the sensory nerves and results in the inhibition of pain. Lignocaine is used in oral preparations in different doses and formulations.21, 22, 23
Cetyl Pyridinium Chloride
It is a quaternary ammonium antiseptic with an antimicrobial effect against gram-positivebacteria and, to a lesser degree, gram-negative bacteria. It increases the permeability of microbial cell membranes to ions and metabolites, which induces a loss of cellular enzymaticand metabolic material, including deoxyribonucleic acid. In addition to its antibacterial activity, CPC also inhibits the growth of some fungi and viruses.24, 25
Cationic quaternary ammonium compounds have antimicrobial properties. Their antibacterial activity is associated with the positive charge of the molecule (cation). The structures of the quaternary ammonium compounds are related to ammonium chloride (NH4Cl).26 The cationic part of the molecule stimulates binding to the anionic compound on the surface of bacteria and may affect the integrity of the cytoplasmic membrane. Once the cytoplasmic membrane is damaged, the functions that involve membrane permeability are affected. The inactivation of the cytoplasmic membrane enzymes has serious consequences, such as protein denaturation. Cationic detergents (quaternary ammonium compounds) are widely used as surface active agents.24, 25, 26
Materials and Methods
This was a single-centre, single blinded clinical case study comprising 10 patients. The study duration was 7 days. The study protocol was initially submitted to the Ethical Committee of the Indraprastha Dental College, Ghaziabad India. After ethical approval was granted, subjects were selected from the outpatient section of the Department of Oral Medicine and Radiology, the Indraprastha Dental College after a written informed consent was taken from them.
The participants in the study group were given the ulcer healing gel and asked to use it for a period of 7 days. Patients were given oral hygiene instructions. Patients were instructed to apply the gel to the ulcer three times a day (after meals and before bedtime) for 7 days using finger or cotton tip applicator and to refrain from eating and drinking for 30 min after application. No other medications were allowed during the study.
Clinical evaluation done at baseline, 3 days, 7 days.
Inclusion criteria
Patients in good health in age range 18– 50 yrs.
Patients in whom oral ulcers / mucosal injuries (epithelial discontinuity are clinically ascertained.
Patients willing to participate in the study and to sign an informed consent form along with having an understanding of all possible risks, aim and methodology of study.
Non-Smokers.
Non-drinkers.
Exclusion criteria
Patient with coagulopathies / bleeding disorders
If subjects are found to be allergic to any ingredients used in study or exhibited any gross oral pathology, eating disorders, chronic disease, pregnancy & lactation, acute myocardial infarction within the past 6 months, use of pacemaker, uncontrolled metabolic disease, major psychiatric disorder, heavy smoking / alcohol abuse, carcinoma's.
Drug hypersensitivities or local irritating factors that could lead to lesion appearance as sharp cusps, improper fillings etc.
Patients who used any treatment for their ulcers 48 h before the start of the study or those who received medications within the last month that can affect the results (e.g., steroids, non-steroidal antiinflammatory, antibiotics).
Parameters for clinical evaluation
Parameters studied included ulcer size, pain scale, erythema, and exudation levels. They were evaluated on baseline (day 0) and at each following evaluation (days 3 and 7).
The ulcer size was determined by measuring the distance between two opposite edges of the ulcer border, using a periodontal probe in millimeters. The surface area of the ulcer is the product maximum ulcer diameter and the measurement perpendicular to it.
Pain intensity scores was evaluated, after irritating the ulcer with the periodontal probe, using a visual analog scale (VAS) consisting of a 10-cm horizontal line between extremities with (0) indicating no pain and (10) for unbearable pain.
Erythema and exudation scores are to be evaluated on a 4-point scale ranging from 0 to 3 based on the method of Greer et al.
Each participant is to be evaluated at each visit by the clinical investigators concerning the emergence of any adverse events, if any, and their relationship to the applied gel.
Results
Table 2
Descriptive data of change in Ulcer Size, Pain Intensity, Erythema and Exudation Scores at different interval of time after use of ulcer gel
Table 3
Descriptive data of change in Ulcer Size, Pain Intensity, Erythema and Exudation Scores at different interval of time after use of ulcer gel
Table 4
Percentage change in clinical parameters over 7 days
| Variable | Baseline- 3 days | Baseline-7 Days |
| Ulcer Size | 51.3% | 88.1% |
| Pain Intensity | 77.4% | 100% |
| Erythema | 43.2% | 85.8% |
| Exudation | 100% | 100% |
The graph showed highly significant reduction in ulcer size, pain intensity, erythema after 7 days and exudation significantly reduced to 100% by 3rd day on usage of ulcer gel. Hence the ulcer gel showed high efficacy.
Discussion
Diagnosis and management of ulcers constitute common problems in dental practice. In the present study, a newly formulated muco-adhesive gels with hyaluronic acid and CPC, lignocaine as active ingredients, has been used as topical therapy for ulcers.13
Hyaluronic acid (HA) is a naturally occurring non- sulfated glycosamino glycan with a high molecular weight of 4000-20,000,000 Da. The structure of HA consists of polyanionic disaccharide units of glucuronic acid and N-acetyl glucosamine connected by alternating bl-3 and bl-4 bonds. It is a linear polysaccharide of the extracellular matrix of connective tissue, synovial fluid, embryonic mesenchyme, vitreous humor, skin, and many other organs and tissues of the body.14, 16
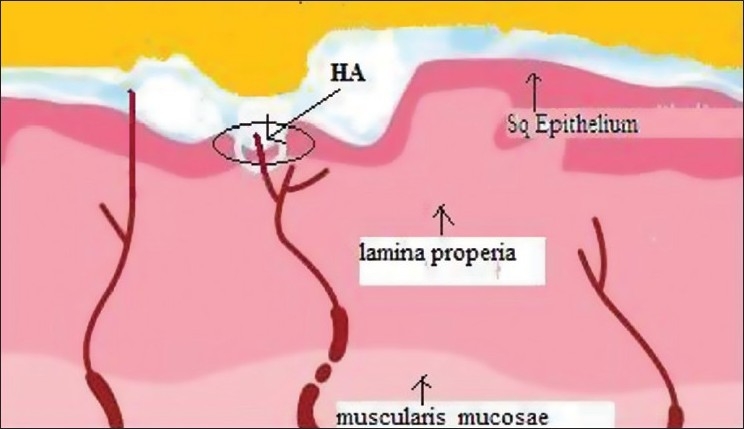
HA is a key element in the soft tissues. It has many structural and physiological functions within these tissues. It can play a regulatory role in inflammatoryresponse: the high-molecular-weight HA synthesized by hyaluronan synthase enzymes in the mucosal. It supports the structural and homeostatic integrityof tissues regulating osmotic pressure and tissue lubrication.23, 24, 25
HA is one of the most hygroscopic molecules known in nature. When HA is incorporated into anaqueous solution, hydrogen bonding occurs between adjacent carboxyl and N-acetyl groups; this feature allows HA to maintain conformational stiffness and to retain water.22
HA also presents important viscoelastic properties reducing the penetration of viruses and bacteria into the tissue. The molecule is also a key component in the series of stages associated with the wound-healing process in both mineralized and non-mineralized tissues - inflammation, granulation tissue formation etc, epithelium formation, and tissue remodeling. As a consequence of the many functions attributed to HA, advances have been made in the development and application of HA-based biomaterials in the treatment of various inflammatory conditions tissues.27, 28, 29
CPC-containing oral products are indicated for uses aimed at preventing and controlling biofilms and inflammation. Choices of CPC concentration may lead to different patterns of effectiveness. CPC is a quaternary ammonium compound that has the ability to reduce bacterial load and the subsequent inflammation.11, 12, 13
Cetylpyridinium chloride (CPC) is an amphiphilic quaternary compound with a long history of safe and effective use when incorporated into oral hygiene products (Haps et al. 2008). This molecule’s positive charge facilitates binding to negatively charged bacterial surfaces (Lim and Mustapha 2007) and, consequently, its antimicrobial activity (Pitten and Kramer 2001). Clinical studies ranging in length from short-term exposure to six-month duration indicate that CPC reduces dental plaque and gingivitis (Allen et al. 1998; Hernandez-Cott et al. 2009; Lotufo et al. 2009; Silva et al. 2009). CPC is categorized by the United States Food and Drug Administration as class I for safety and class I for efficacy (2003).
Recent research indicates that CPC diffuses into oral biofilms irrespective of the thickness of extracellular components and appears to bind irreversibly (Sandt et al. 2007). In studies with streptococcal glucosyl transferases (Furiga et al. 2008) and fructosyl transferases (Steinberg et al. 2002), CPC inhibits insoluble glucan synthesis. The solubility profiles of CPC facilitate its incorporation into mouthwashes, lozenges (Taylor et al. 1997), varnishes (Steinberg et al. 2001) and mucoadhesive patches or gels (Nafee et al. 2003; Lee et al. 2008).
The effect of HA and CPC produced an enhanced healing efficacy and reduction in inflammation at the ulcer site. The erythema and exudation were reduced to about 86% and 100% respectively in comparison to the baseline scores. As a result of reduced inflammation and fastened healing the pain reduction was also seen to be statistically significant at the ulcer sites.
Lignocaine alone or in combination with another local anaesthetic is a well-known product for local pain reduction.12
The clinical data obtained in this study trial showed that topical application of the gel containing Lignocaine gel for 7 days to the ulcers wounds produced a significant reduction in pain intensity after application that the pain reduction was statistically significantly over a period of 3 days and 7 days when compared to baseline. The pain decreased by approximately 77% after 3 days and about 100% after 7 days. The lidocaine containing gel did not elicit any negative side effects.
Xylitol 2% also present as a constituent contributes to the antibacterial activity of the gel and due to its sweet nature being a type of sugar, also adds to the palatability of the gel in the oral cavity. First, it interferes with the bacterial growth and its ability to produce acid. Second, it blocks communication between bacteria so they stop producing the polysaccharide slime that holds the biofilm together. Third, it raises the pH of the mouth.
Conclusion
In conclusion, we suggest that the current gel approach offers an effective therapy for oral ulcers. Both HA and CPC in combination with xylitol and lignocaine proved to be effective in management of ulcers providing relief in as early as 3 days. HA, CPC was superior in decreasing ulcer size, erythema, and exudation; whereas Lignocaine resulted in faster pain reduction. The fact that no side effects were encountered with the use of the muco-adhesive gel supports the safety of this gel formulation.