- Received March 09, 2022
- Accepted March 14, 2022
- Publication July 22, 2022
- Visibility 11 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijohd.2022.008
-
CrossMark
- Citation
Utility of lasers in orthodontics
- Author Details:
-
Princy Garg *
-
Sonali Bhatt
-
Vedika Joshi
-
Tarun Kumar
Introduction
The name “LASER” stands for “Light Amplification by Stimulated Emission of Radiation”. A laser can produce light by transforming electrical energy into optical energy. To generate laser light, atoms must be excited to a higher energy level and release their energy in phase.
Laser, as defined by 3 properties is monochromatic, directional and coherent. These properties are different from ordinary light which is non-coherent and diffuse.[1]
Albert Einstein was the first who proposed the theory of “Stimulated emission” as early as 1917.Physicist Theodore H. Maiman in 196O was the first to develop the first laser to use visible light which used a ruby medium[2] after the theoretical study by Einstein, Townes, Prokhorov and Basov.[3]
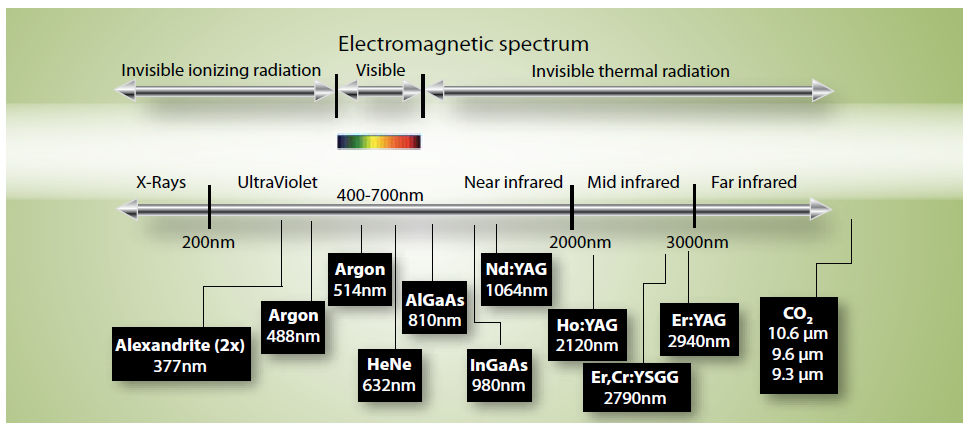
The range of the wavelength of lasers employed in dentistry is 488 nm and 1O,6OO nm. ([Figure 1]).[4] The lasers used in dentistry are the:-
CO2 laser
Argon laser
Neodymium-doped Yttrium Aluminum Garnet (Nd: YAG) laser
Erbium lasers [Erbium-doped solid state lasers].
Diode laser
These lasers are termed according to their suspension state and active medium content.[5]
Advantages of Laser Excision vs. Scalpel Surgery
Compared to conventional scalpel surgery there are numerous advantages of laser. The most significant of them all is the clear field provided by it due to coagulation of blood vessels and sealing off lymphatics during ablation. Also the cut by the laser is more accurate also laser has an additional benefit of sterilizing the surgical field while ablation. Laser surgery is performed using only compound topical anaesthetic or light anaesthetic studies also suggest that less scar tissue is produces with laser as compared to scalpel. Shorter operating time with lasers is an undeniable advantage for the busy practitioner. Discomfort and pain experienced by the patients post surgically is significantly less when the procedure is done with laser.[6]
Lasers for Soft Tissue Procedures
The most commonly used soft tissue lasers include the:[6], [7]
CO2 (1O,OO nm),
Diode lasers (800–980 nm)
Argon laser
Erbium solid state lasers (Erbium-doped yttrium-aluminium-garnet [Er:YAG] laser (2,940 nm).
Neodymium-doped yttrium-aluminium-garnet [Nd:YAG] laser (1,064 nm)
Potassium, Titanium and Phosphate [KTiOPO4, KTP] laser (532 nm)
Clinical Application of Laser in Orthodontics
Numerous common applications of lasers in orthodontic practice includes accelerated tooth movement, ceramic brackets debonding, etching of enamel prior to bonding and pain alleviation post orthodontic force and prevention of demineralization of the enamel, frenectomy, operculectomy, minor apthous ulceration ablation, tooth and mini-implant exposure etc.[8]
Etching of Enamel Prior to Bonding
After laser irradiation, changes such as recrystallization and melting take place in enamel, leading to the occurrence of innumerous pores and bubble-like inclusions.[9] Due to this, laser radiation is a suitable method for etching of enamel. Additionally, it is reported that etching by laser results in the fractured, open dentin tubules and uneven surface, which is ideal for adhesion.[10]
Aesthetic Laser Gingival Recontouring
Dental aesthetic procedures like papilla flattening or aesthetic crown can be technically demanding tasks as gingival margins sometimes need very minor recontouring that needs a higher degree of precision that is difficult to be attained with a scalpel blade, regardless of the operator’s skill level. Diode lasers offer the accurate incision control because of reduced bleeding and a clear dry field during surgery.([Figure 2], [Figure 3])[11]


Enamel Decalcification Reduction
As suggested by numerous studies, laser can be used to avert decalcification of enamel at the subsurface by changing its crystalline structure, permeability and acid solubility[13], [14], [15], [16] although it should be used at low intensity to prevent the enamel disintegration. Richard et al.[14] studied the efficacy of Argon laser irradiation to lessen the demineralization and loss of structure of tooth in vivo. In the mentioned study, a 250 mW argon laser at 12 J/cm2 is used on the experimental teeth before banding and they showed a reduction of 29% in demineralization in comparison to the control teeth.
Alleviating Pain Post Orthodontic Force Application
Pain and discomfort is felt by the patient for two to four days after application of orthodontic force “Low-level laser therapy (LLLT)” can be used as an analgesic management for orthodontic treatment. LLLT also acts on biostimulating process of repairing the tissues. In this, the output of energy is low enough to intercept the temperature rise above 36.5°C in the target tissue.[17], [18], [19]
Soft-Tissue Applications of lasers for Orthodontic Treatment
During soft-tissue incision, dental lasers allow convenience and precision. Lasers:
Cause least damage of tissue,
Provide hemorrhage control
Post-operative pain reduction.
Soft tissue applications of dental lasers associated with orthodontic treatment include exposing partially erupted and unerupted teeth, gingival contouring, hypertrophic or inflamed tissues removal, frenectomy and management of aphthous lesions.[20] Other uses include aesthetic contouring of the gingiva, creating proper tooth proportionally before bracket bonding, crown lengthening procedure, managing asymmetry of crown height or gingival margins and interdental margins contouring.[21] Nd solod state lasers are used particularly for soft-tissue uses such as flattening of papilla, frenectomy, gingivectomy etc.
Accelerating Orthodontic Tooth Movement
As compared to other methods like corticotomy of pharmacologic interventions, lasers provide the better alternative with reduced side-effects for accelerating orthodontic tooth movement to achieve faster completion of the treatment. “low level laser therapy” is used for this purpose. It induces the biostimulatory response in the adjacent periodontal ligament tissue. The most important factor which determines the tooth movement is the bone remodelling in the periodontal tissue affected by various factors. LLLT enhance the movement by stimulating the OPG/RANK/RANKL.[22], [23]
Debonding of Ceramic Brackets
Due to brittle nature, high bond strength and lower fracture toughness of ceramic bracket, debonding of these brackets leads to enamel fracture. Therefore debonding od ceramic brackets is difficult as compared to metal brackets. To conveniently debond the ceramic brackets, lasers can be used as they change the bond strength between the bracket and the tooth. The adhesive is softened with laser irradiation and hence debonding can take place in 1-5 seconds. Neodymium and erbium solid state laser, diode laser and co2 lasers are efficient for the purpose of debonding of polycrystalline and monocrystalline ceramic brackets.[24]
Other utility of the Laser for Soft Tissue Procedures in Orthodontics
Numerous other soft tissue procedures that can be done with the help of lasers include: [21], [25], [3]
Frenectomy
Uncovering the ‘temporary anchorage devices’ (TADs)
Operculectomy
Uncovering impacted tooth
Management of minor aphthous ulcers
Requirements and Recommendations for Laser Safety[4]
Warning sign representing the laser is in use.
Using protective goggles by patient as well as the operator
Reflective surfaces like table, jewellery or belt should be minimized
High-volume suction should be used
Sterilization protocols should be followed
Presence of laser safety officer
Informed consent
Adequate training of the user
Potential fire hazards should be considered
Conclusion
Incorporating lasers in the field of orthodontics leads to efficacy in the overall management of the patient. Reduced pain and discomfort following the treatment is the major factor for the patient’s overall comfort. Also patient can be benefitted by minimizing the total treatment time. Reduced blood and clear visibility of the surgicial field during the procedure helps the operator in providing much precise treatment and aesthetically laser pleasing results. Reduced treatment time also helps to increase the efficiency of the practitioner. However inherent risks should be recognized so that to avoid any potential injury.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
References
- Y Kang, AB Rabie, RW Wong. A review of laser applications in orthodontics. Int J Orthod Milwaukee 2014. [Google Scholar]
- TH Maiman. Stimulated Optical Radiation in Ruby. Nature 1960. [Google Scholar]
- ND Kravitz, B Kusnoto. Soft-tissue lasers in orthodontics: an overview. Am J Orthod Dentofacial Orthop 2008. [Google Scholar]
- D Roberts-Harry. Lasers in Orthodontics. Br J Orthod 1994. [Google Scholar]
- LJ Miserendino, EJ Neiburger, RM Pick. Current status of lasers in dentistry. Illinois Dent J 1987. [Google Scholar]
- A Aoki, K Mizutani, F Schwarz, A Sculean, RA Yukna, AA Takasaki. Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000 2015. [Google Scholar]
- P Pang, Andreana S Aoki, A Coluzzi, D Obeidi, A Olivi, G Parker, S Rechmann, P Sulewski, J Sweeney, C Swick, M. Laser energy in oral soft tissue applications. J Laser Dent 2010. [Google Scholar]
- R Nalcaci, S Cokakoglu. Lasers in orthodontics. Eur J Dent 2013. [Google Scholar]
- LM Silverstone, CA Saxton, IL Dogon, O Fejerskov. Variation in the pattern of acid etching of human dental enamel examined by scanning electron microscopy. Caries Res 1975. [Google Scholar]
- SR Visuri, JL Gilbert, DD Wright, HA Wigdor, JT Walsh. Shear strength of composite bonded to Er: YAG laser-prepared dentin. J Dent Res 1996. [Google Scholar]
- EA Lee. Laser-assisted gingival tissue procedures in esthetic dentistry. Pract Proced Aesthet Dent 2006. [Google Scholar]
- A Borzabadi-Farahani, M Cronshaw, D Coluzzi, S Parker. Lasers in Orthodontics. Lasers in Dentistry—Current Concepts. Textbooks in Contemporary Dentistry 2017. [Google Scholar]
- AM Anderson, E Kao, M Gladwin, O Benli, P Ngan. The effects of argon laser irradiation on enamel decalcification: An in vivo study. Am J Orthod Dentofacial Orthop 2002. [Google Scholar]
- RJ Blankenau, GL Powell, RW Ellis, GH Westerman. In vivo caries-like lesion prevention with argon laser: pilot study. J Clin Laser Med Surg 1999. [Google Scholar]
- T Oho, T Morioka. A possible mechanism of acquired acid resistance of human dental enamel by laser irradiation. Caries research 1990. [Google Scholar]
- L Noel, J Rebellato, RD Sheats. The effect of argon laser irradiation on demineralization resistance of human enamel adjacent to orthodontic brackets: an in vitro study. Angle Orthod 2003. [Google Scholar]
- T Fukui, M Harazaki, K Muraki, T Sakamoto, Y Isshiki, H Yamaguchi. The evaluation of laser irradiated pain reductive effect by occlusal force measurement. Orthod Waves 2002. [Google Scholar]
- HM Lim, KK Lew, DK Tay. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofacial Orthop 1995. [Google Scholar]
- S Saito, Y Mikikawa, M Usui, M Mikawa, K Yamasaki, T Inoue. Clinical application of a pressure-sensitive occlusal sheet for tooth pain-time-dependent pain associated with a multi-bracket system and the inhibition of pain by laser irradiation. Orthod Waves 2002. [Google Scholar]
- DM Sarver, M Yanosky. Principles of cosmetic dentistry in orthodontics: Part 3. Laser treatments for tooth eruption and soft tissue problems. Am J Orthod Dentofacial Orthop 2005. [Google Scholar]
- DM Sarver, M Yanosky. Principles of cosmetic dentistry in orthodontics: Part 2. Soft tissue laser technology and cosmetic gingival contouring”. Am J Orthod Dentofacial Orthop 2005. [Google Scholar]
- MC Walsh, Y Choi. Biology of the RANKL-RANK-OPG System in Immunity. Front Immunol 2014. [Google Scholar] [Crossref]
- S Fujita, M Yamaguchi, T Utsunomiya, H Yamamoto, K Kasai. Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthod Craniofac Res 2008. [Google Scholar]
- K Hayakawa. Nd: YAG laser for debonding ceramic orthodontic brackets. Am J Orthod Dentofacial Orthop 2005. [Google Scholar]
- LG Chmura, RA Convissar, RA Convissar. Lasers in orthodontics. Principles and practice of laser dentistry 2016. [Google Scholar]
- Introduction
- Advantages of Laser Excision vs. Scalpel Surgery
- Lasers for Soft Tissue Procedures
- Clinical Application of Laser in Orthodontics
- Etching of Enamel Prior to Bonding
- Aesthetic Laser Gingival Recontouring
- Enamel Decalcification Reduction
- Alleviating Pain Post Orthodontic Force Application
- Soft-Tissue Applications of lasers for Orthodontic Treatment
- Accelerating Orthodontic Tooth Movement
- Debonding of Ceramic Brackets
- Other utility of the Laser for Soft Tissue Procedures in Orthodontics
- Requirements and Recommendations for Laser Safety[4]
- Conclusion
- Source of Funding
- Conflict of Interest
