- Visibility 1.5k Views
- Downloads 73 Downloads
- Permissions
- DOI 10.18231/j.ijohd.2020.038
-
CrossMark
- Citation
Periodontal diseases- A brief review
- Author Details:
-
Pragati Dubey *
-
Neelam Mittal
Abstract
Periodontal diseases consists of a wide range of inflammatory conditions which causes degeneration of Periodontium and affects all supporting structures of teeth such as gingiva, periodontal ligament, cementum and alveolar bone etc. followed by teeth loss. WHO had reported about 10-15% of the world population is suffering from severe periodontal condition. It is complex infectious disease caused by aggressive microbial growth on teeth. The main aim of this study is to provide systemic update on periodontal disease regarding its stages, occurrence, pathophysiology, diagnosis, treatment and management. The pathophysiology of periodontal disease is associated with dental plaque, microbial biofilm formation and immunogenicity of the host cell. The severity of this disease depends upon risk factors and chronological stages. Prevention is attained by daily maintenance of oral hygiene. Various surgical and non-surgical treatments are available to control the formation of microbial biofilm. Daily maintenance and periodic management of this disease control worsening of condition and shows definite improvement in oral health.
Background
Periodontitis is an infection of Periodontium. Whereas, the word ‘Perio’ means gingiva and other tissues surrounding teeth, ‘dont’ mean tooth and ‘itis’ means inflammation, So the whole term “Periodontitis” indicates chronic inflammation of gingiva[1] periodontal ligaments, alveolar bone and dental cementum. According to World Health Organization (WHO) it is widely spreadable chronic disease around the world.[2] It begins with accumulation of plaque around teeth which form microbial biofilms with bacteria followed by localized inflammation of gingiva. Negligence of this situation causes chronic condition of periodontal disease. At this stage damage of periodontal structure occurs by baleful byproducts and enzyme from periodontal bacteria such as leucotoxins, collagenase, fibrinolysis and other Bacteroids spp.: B. intermedius and B. gingivalis, fusiform organisms: Actinobacillus actinomycetemcomitans, Wollina recta and Eikenella spp.; Porphyromonas gingivalis, Taneerella for synthesis and various bacilli and cocci; spirochetes; and amoebas and trichomonads.[3], [4], [5]
By maintaining good oral hygiene, it can be reversed at initial stage but if plaque is not removed at this stage then formation of tartar or calculus occur which is not removable by using tooth brush or floss. Because of this tartar, bacteria start attacking deeper tissues due to which periodontal ligaments around teeth gets degraded and leads to resorption of alveolar bone.[6] A space between gingiva and tooth occurs which is referred as “Periodontal Pocket” and this condition is mainly known as periodontitis or periodontal disease. The severity of this disease depends upon microbial plaque formation.[7]
The screening and examination of this disease has been done by various methods, which results in detection of severity of periodontal ligament. Several tests are there to diagnose the periodontal disease such as radiograph technique, hematological screening, laser treatment, tissue engineering, etc. To control the progression of disease there are many treatment options available (surgical as well as non-surgical) depend upon the chronology of disease. The maintenance of this disease is done by intensive care and by sustaining good oral hygiene.[8], [9]
Stages
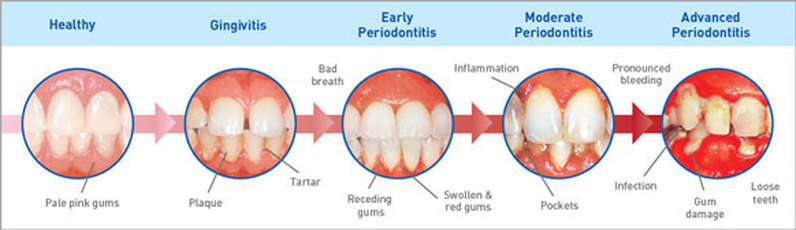
There are mainly four stages in periodontal diseases which includes different clinical sign & symptoms and radiological screening are given as follows:[10], [11], [12]
Gingivitis
It is the only stage when periodontitis can be reversible. At this stage the plaque formation around teeth occurs. There are mainly few painless symptoms seen at this stage such as bad breath, swollen reddish gums and bleeding while brushing and flossing. It can be reversed by maintaining good oral hygiene and regular checkups. Generally, 1-2 mm clinical attachment loss, less than 15% of bone loss around root, probing depth 4mm or less occurs.
Early stage
It is the second stage of periodontal disease. It is manageable by oral hygiene but not reversible. At this stage, the infection starts spreading to surrounding tissues and starts degrading it. Symptoms at this stage include inflammation of gums, severe bad breath, and bleeding during brushing or flossing, spacing between teeth become evident and will gradually increase. Here, 3-4 mm clinical attachment loss, less than 15-33% of bone loss around root, probing depth 5mm or less occurs.
Moderate stage
Like second stage moderate stage cannot be reversed. Same symptoms as moderate stage occurs but space between teeth and recessions of gums are more evident. Treatment like deep cleaning, scaling and flap surgeries can be done at this stage. Around5 mm or more clinical attachment loss, 33% of tooth loss of four teeth or less, with complex issues such as probing depth 6 mm or more, Class II-III furcations, and/or moderate ridge defects.
Advanced stage
Last stage of periodontal disease; wherein 50-90% of loss of periodontal tissues occurs. Also other symptoms like swollen gums that ooze of pus, cold sensitivity, loosening of teeth, painful chewing and severe halitosis occurs. If left untreated it causes more spaces or gaps between teeth and gums, gum recession, patient needling dentures, and other health problems that can be worst. Treatment includes regular checkups, cleaning and maintaining good oral hygiene can help halt the progression of Periodontitis. Secondary Occlusal trauma, severe ridge defects, bite collapse, pathologic migration of teeth, less than 20 remaining teeth (10 opposing pairs) seen.

Types of Periodontitis[15], [16], [17], [18]
Gingivitis
As described above, gingivitis is inflammation of gums and can be reversed by maintaining oral hygiene.
Chronic periodontitis
In this type of periodontal disease, symptoms may include chronic inflammation of gums, severe bad breath, and bleeding during brushing or flossing occurs. Loss of epithelial tissue, bone and ligaments which is not reversible.
Aggressive periodontitis
It can be present in localized or generalized forms, both are early onset form of chronic periodontal inflammatory disease, typical manifesting between puberty and early third decade of life. The symptoms are same as chronic periodontitis.
Necrotizing ulcerative gingivitis
It is mainly occurring in people who are suffering from malnutrition, immune suppressive and HIV. Necrosis means death of cell or living tissue. It mainly occurs due to deficiency of nourishment needed by people to remain healthy.
Peri-implant mucositis
It is associated with inflammation of soft tissue surrounding dental implants with no sign of bone loss. Symptoms included red or tender gums around implants, bleeding while brushing.
Systemic chronic periodontitis
This type of chronic periodontal disease happens in patient who have systemic syndrome. Inflammation of gums occurs due to systemic disease such as Diabetes, Heart disease, Respiratory disease, etc.

Occurance & Epidemiology
Periodontal disease is mostly prevalent in adults but it may also occur in children and adolescents.[20] Prevalence of periodontal diseases depends upon the level of dental plaque formation and gingival tissue destruction. Site specificity is one of the key features for chronic and aggressive periodontitis. The severity of this disease depend upon depth of periodontal pocket i.e. attachment loss and bone loss of tooth.[21]
The epidemiology of periodontitis may vary across masses substantially. Frequently used parameters to collect data for occurrence of this disease are clinical attachment loss and probing depth of periodontal pockets which was first introduced by US centers for Disease Control Prevention and American Academy of Periodontology.[22]
Various studies were conducted by researchers to find out prevalence rate in different countries. Globally 10-15% of populations are suffering from tooth loss due to periodontal disease.[23] A study was conducted in Gautemala by Dowsett et al in 2001 reported that out of 122 patients, attachment loss was found about 3 and 6 mm in 100% and 56% of overall individuals respectively.[24] Afterwards in 2003, another clinical study by A. Baelum et al. reported that out of 359 patients of rural Thai population, 92% were diagnosed with higher prevalence of periodontitis due to genetic variation within age group of 30-32 years individuals.[25] Also in 2017, another study was conducted in South India among 1000 individuals which showed prevalence rate of chronic periodontitis among different strata of sample populations ([Table 1]).[26] Similarly, another clinical study conducted by researchers in 2018 about prevalence rate of periodontitis among different age group of people of South India ([Figure 4]).[27]
| Population | Periodontitis prevalence (n=1000) | Prevalence percentage n (%) |
| Male | 252 | 42.4 |
| Female | 171 | 42.1 |
| Hypertension | 19 | 44.2 |
| Diabetes Type-II | 25 | 43.9 |
| Cigarette smoking | 53 | 44.9 |
| Alcohol consumption | 60 | 39.7 |
| Pan chewing | 35 | 43.2 |

Risk factor
There are two kind of risk factor in case of periodontal disease out of which one is modifiable and another is non-modifiable.[28] Cigarette smoking is one of the vital modifiable risk factor for chronic periodontal disease. Higher progression of microbial film is severe in smokers than nonsmokers and more worsen chronic condition occurs due to habit of smoking.[29] Most prevalent systemic disease is diabetes mellitus predispose to periodontitis. In diabetic patient, prevalence of periodontitis occurs more readily as compared to other immunocompromised patients.[30] Stress is also another consideration as immunosupression and necrotizing ulcerative gingivitis occurs mainly due to stress.[31] There are many risk factors associated with this disease are given as ([Table 2]).
| Modifiable risk factor | Non-modifiable risk factor |
| Microorganisms (specific pathogen) | Osteoporosis |
| Smoking | Some hematological disorders |
| Poorly controlled diabetes mellitus | History of periodontitis |
| Stress | Age |
| Poor self-care | Gender |
| Untreated human immunodeficiency virus or acquired immunodeficiency syndrome | Race |
| Oral effects of some metabolism | Genetic disorders |
| Local factors | Bone level |
| Obesity | Drug-induced disorders |
| Improper diet | Some host response |
| Chronic inflammation | Bone levels |
| Some host responses | Normal hormonal variations (e.g. pregnancy) |
Pathophysiology
The dental plaque or calculus
Periodontitis and gingivitis are mainly initiated with dental plaque. There are around 150 species of microbes are found in single person and overall 800 different types of species of microbes have been identified in calculus of tooth. The species include Gram negative anaerobic bacteria, spirochete and even virus. The imbalance between these microbes forms ‘pathogenic unit’ in case of chronic periodontal disease.[32]

Microbial biofilms
As we discussed earlier, microbial biofilm initiates gingivitis. The progression of microbial biofilm depends upon dysbiotic ecological changes in baleful byproducts and enzyme which results in degradation of periodontal tissue. Microbial biofilms are kind of matrix fixed with different microbial species colony, sticking with each other on tooth surface.[34] There are seven stages of plaque biofilm formation are given as ([Table 3]).
| No. | Stages | Features |
| 1 | Pellicle formation | Occurs by adsorption of Host and bacterial molecules, salivary glycoprotein on tooth surface. |
| 2 | Transport | Occurs via natural salivary flow, transport of bacteria such as Neisseria, Streptococcus sanguis, S. oralis, S. mitis and Actinomyces to the pellicle occurs. |
| 3 | Long range interactions | This stage leads to reversible adhesion with Vander Wall’s and electrostatic forces between microbial cell surface and the pellicle. |
| 4 | Short range interactions | This stage leads to irreversible interaction between microbial cell surface and pellicle. |
| 5 | Co-aggregation | Increased micro flora diversity due to co-adhesion of new microbes over already attached microbes. |
| 6 | Multiplications | Multiplication of adhered bacteria on tooth surface lead to severity of periodontal disease. |
| 7 | Detachments | Detachment of colonies to the new site for confluent growth. |
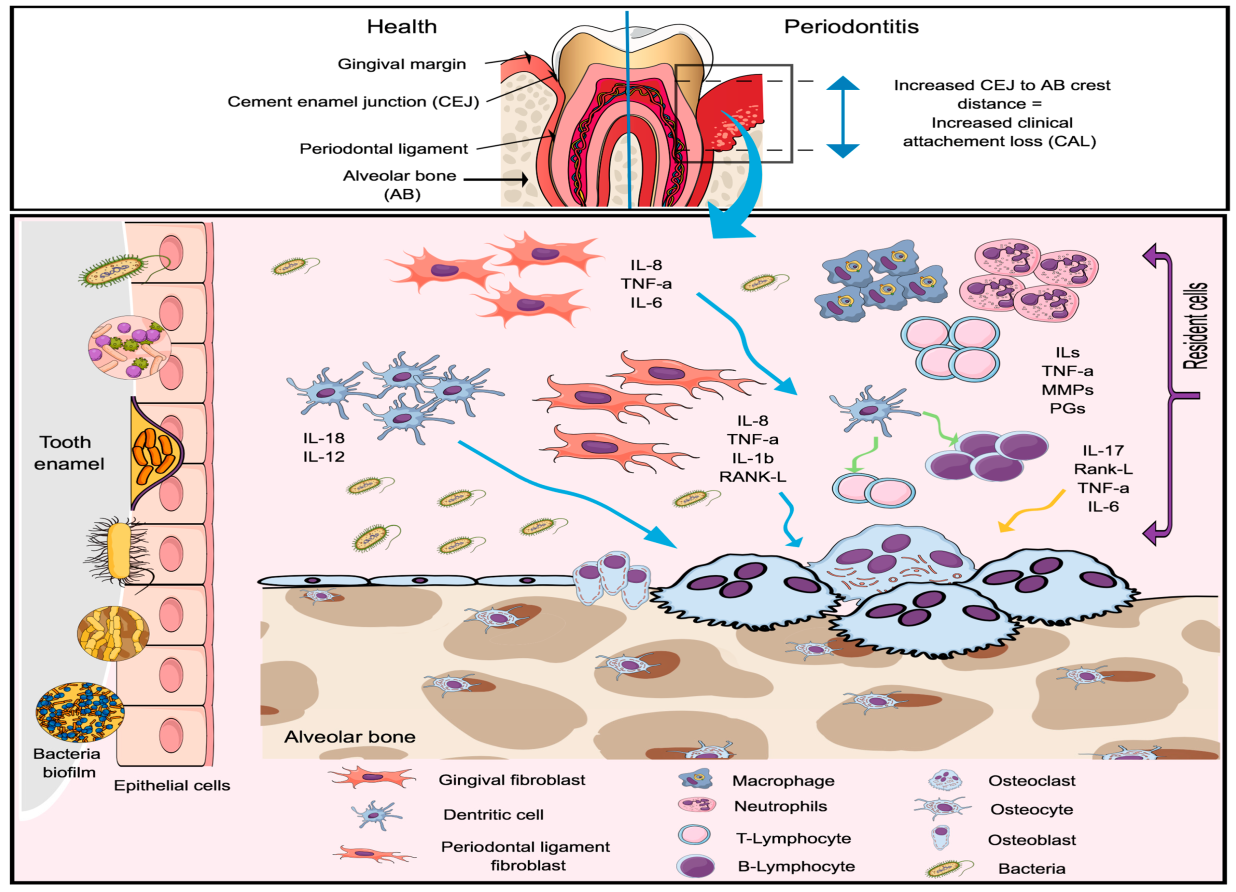
Immunogenicity
Not only microbial films are responsible for pathogenesis of periodontal disease but also host cells immune system is responsible for degradation of periodontal ligaments.[36] The balance between microbial biofilm and host cell is lost due to which remarkable variance in both dental plaque and host immunity system occurs, which results in increment of inflammatory cells leads to degradation of periodontal tissue and bone.[37] Therefore decrease of anti-inflammatory cells such as neutrophils, lymphocytes, granulocytes, etc. due to chronic persistence of microbial biofilms which results in severity of alveolar bone resorption by osteoclast and leads to degradation of ligament fibers followed by chronic periodontitis.[38]
Periodontal Screening and Examination[40], [41]
The dental examination starts with an extra cellular and intra cellular oral examination of soft and hard tissues. The periodontal examination includes these following steps as follows:
General description like
Quantitative assessment of oral hygiene and presence of calculus deposits.
Presence of gingival inflammation and recession.
Tooth migrating and related problems.
Identification of local periodontal risk factors.
Periodontal screening using basic periodontal examination and recordings
Detailed examination of ligament degradation and periodontal pocket depth as:
Probing depth of periodontal pocket, attachment loss and recession
Bleeding.
Suppuration.
Furcation involvement.
Mobility of tooth.
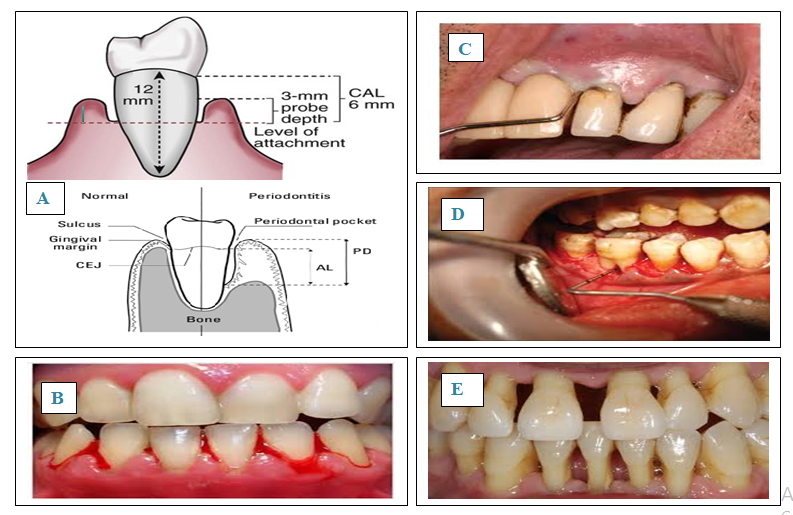
All these parameters are measured on six sites per tooth such as mesiobuccal, buccal, distobuccal, mesiolingual, midlingual and distolingual. And all these readings are recorded in periodontal chart.
Diagnosis[45], [46], [47]
Diagnosis of periodontal disease has been done by following investigations are given as:
Radiograph
Periapical radiograph, Bitewing radiographs, Panoramic X-ray or combination of all these is used to diagnose the prognosis of patients.
Radiograph provides detailed information about patient’s tooth condition. The degree of bone loss and depth of periodontal pocket can be assessed by using Radiograph and also pattern and amount of bone loss.
| Radiograph types | Parameters |
| Periapical radiograph | • Long cone parallel technique.• Good clarity of images as compared to horizontal radiograph.• Time consuming process. |
| Horizontal bitewings radiograph | • Use for caries detection. • Alveolar crest can be visualized. • Provides good quality of image for bone loss. |
| Vertical bitewing radiograph | • Shows 90° angle bitewing film image. • Better quality of image for extensive bone loss |
| Panoramic radiograph | • All teeth seen in one image or film. • Newer machine generated for good quality of images. • Details are much fine as compared to intraoral radiographs. |
Vitality test
Electric Pulp tester or Thermal stimuli is used to diagnose the pulp vitality of tooth.
Other tests
Full hematological screening.
Blood glucose level test.
INR or microbial plaque sampling
Treatment and Management
Treatment plan for periodontal disease are divided into three phases as follows:
Initial therapy
This therapy is given at initial stage of gingivitis to control the microbial plaque formation and identify any modifiable risk factor.[48] Giving advice to the patients regarding oral hygiene technique, cessation of habits like smoking, alcohol consumption, chewing pan masala, etc. and also doctors gives instruction regarding type of toothbrush to be use, use of interdental aids, dentifrices or mouthwash, etc.[49] If periodontal risk factors like Diabetes mellitus identified then patient should be advised accordingly. The therapy is revaluated after 8-12 weeks because 6 weeks is minimum period for healing of tissue or periodontal ligaments. The initial treatment includes following therapies:
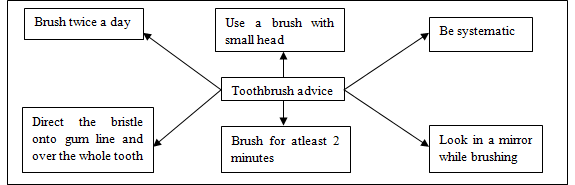
Tooth brushing
Manual and electronic toothbrush are available to remove dental plaque. Robinson et al in 2005 reported in this study that oscillating, rotating, powered toothbrush shows more efficiency in removing dental plaque.[50]
Interdental cleaning
An effective toothbrush can clean only 65% of tooth surface but do not remove overall dental plaque, so interdental cleaning is also necessary to clean the microbial biofilms such as dental floss, tape and powered flossing device. When interdental papillae completely embrasure then dental floss and tape are advised to the patient which helps to improved periodontal clinical outcomes.[51] ([Figure 9] )
Adjunctive pharmacological agent
Many Pharmaceutical aids have been added into mouthwashes and toothpaste to increase the efficiency of the product. Widely used agent like Chlorhexidine Gluconate is considered as gold standard anti-plaque/ anti-gingivitis agent.[52] It is mainly added into mouth wash, gel or toothpaste. There are various examples of adjunctive aids are given as ([Table 5]).
| Compounds | Pharmacological aids |
| Bisguanidine | Chlorhexidine gluconate |
| Enzyme | Protease, dextranase |
| Quaternary ammonium compounds | Cetyl pyridinium chloride |
| Phenols | Triclosan |
| Essential oils | Thymol, eucalyptol |
| Metal ions | Zinc, stannous fluoride |
| Oxygenating agents | Peroxide |
Non-surgical treatment:[53], [54]
At initial stage of gingivitis, the treatment may be less aggressive as given as:
Scaling
Scaling helps to remove calculus and microbial biofilms from gums. It may be operated by using hand instruments or by ultrasonic device.
Root planning
Root planning helps to smooth the root surface and also inhibiting further buildup of tartar. It also removes baleful byproducts to reduce the inflammation and increase healing of attachment of gums to tooth surface.
Antibiotics
Topical or Oral antibiotics are used to control the formation of microbial biofilms. Topical antibiotics such as insertion or gels or implants etc. are inserted in gingival sulcus or in periodontal pockets. However, Oral antibiotics eliminate infection caused by bacteria on gums and teeth surfaces.
| No. | Surgical Treatments | Features |
| 1. | Flap surgery | • Pocket reduction surgery. • Incision on gum tissue for better healing. |
| 2. | Soft tissue grafting | • Removal of small tissue from palate. • Use for reducing gum recession. |
| 3. | Bone grafting | • Bone grafting of small fragment from own, synthetic or donated bone. • Helps in tooth loss problems and regrowth of natural bone. |
| 4. | Tissue-stimulating proteins | • Applying gel to a diseased tooth root. • Gel helps in developing tooth enamel and stimulates growth of bone and tissue. |
| 5. | Reparative surgery | • Modified windman flap technique. • Use for better access and direct vision to root surface of debridement. |
| 6. | Resective surgery | • Gingivectomy. • Removal and reshaping of tissue occur. |
| 7. | Regenerative surgery | • Regeneration of Periodontium. • Regrowth of bone that destroyed by bacteria. • Example as tissue regeneration or enamel matrix derivation. |
| 8. | Other surgery | • Occlusal adjustment. • Endodontitis. • Extraction of microfilm. • Fixed/ Removal prosthodontics. • Implants. • Host modulation therapy. • Orthodontics. • Laser surgery. • Tissue engineering. |
Corrective therapy or surgical treatments[55], [56], [57], [58]
There are several surgical treatments to treat periodontal disease ([Table 6]).
Supportive therapy
This therapy is suggested for prevention of recurrence of disease and also sustenance of periodontal health.[59] This therapy includes regular check-ups of the patient, to monitor the periodontal status and to re-educate to the patient regarding plaque control measures and oral hygiene maintenance.[60]
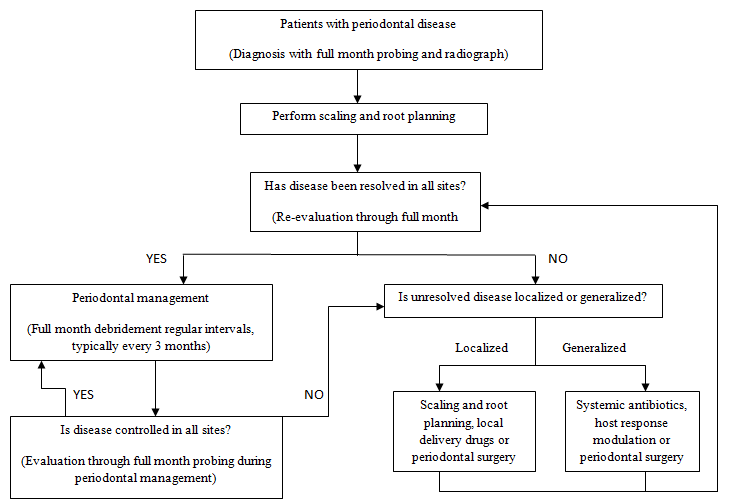
Management: Periodontal disease has capacity to control the progression of disease and inhibit the growth of microorganisms. However, the success of therapy for periodontal disease depends upon appropriate management with proper treatments.[61] The management of periodontal disease consists of removal of supra-gingival and sub-gingival dental plaque followed by healing in tooth loss.[62] In general it takes around 3 months of treatment interval to control the chronicity of periodontal disease. Maintenance period has been customized depends upon severity of disease. Supportive therapy aims long term maintenance of disease, so proper measures are taken to improve the compliances of management by patients to control the disease progression.[63] Management plan for periodontal disease includes [Figure 10].
Clinical Significance
There has been known direct and indirect impact on overall general health due to oral health. This study helps to improve researcher’s knowledge regarding periodontal diseases. Due to rapidly increase of progression and aggressiveness of this disease, patients requires early diagnosis and treatment to prevent from further progression and tissue damage. With the growing advancement in etiopathogenesis of this disease, there have been exponential increments in novel treatment strategies. There are various treatment modalities available for treatment of periodontal diseases. A thorough diagnosis and treatment planning is important for the management of patient to reduce the chronicity of this disease.
Source of Funding
None.
Conflict of Interest
None declared.
References
- Preshaw PM, Bissett SM. Periodontitis: Oral Complication of Diabetes. Endocrinol Metab Clin N Am. 2013;42(4):849-67. [Google Scholar]
- Chapple ILC, Mealey BL, Dyke TEV, Bartold PM, Dommisch H, Eickholz P. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45(S20):24-9. [Google Scholar]
- White D, Pitts N, Steele JG. Diseases and related disorders- a report from the adult Dental Health Survey. NHS Information Centre for Health and Social care. . 2011. [Google Scholar]
- Yucel-Lindberg T, Båge T. Inflammatory mediators in the pathogenesis of periodontitis. Expert Rev Mol Med. 2013;15:7-11. [Google Scholar]
- Abusleme L, Dupuy AK, Dutzan N, Silva N, Burleson JA, Strausbaugh LD. The subgingival microbiome in health and periodontitis and its relationship with community biomass and inflammation. ISME J. 2013;7(5):1016-25. [Google Scholar]
- Nelson RG, Shlossman M, Budding LM, Pettitt DJ, Saad MF, Genco RJ. Periodontal Disease and NIDDM in Pima Indians. Diabetes Care. 1990;13(8):836-40. [Google Scholar]
- Holand C. Rethinking perio classification for the 21st century. BDJ Team. 2019;6(3):24-7. [Google Scholar]
- Savage A, Eaton KA, Moles DR, Needleman I. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J Clin Periodontol. 2009;36(6):458-67. [Google Scholar]
- Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;89(1):1-8. [Google Scholar]
- Fine DH, Patil AG, Loos BG. Classification and diagnosis of aggressive periodontitis. J Periodontol. 2018;89:S103-7. [Google Scholar]
- Dietrich T, Ower P, Tank M, West NX, Walter C, Needleman I. Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions – implementation in clinical practice. Br Dent J. 2019;226(1):16-22. [Google Scholar]
- Graetz C, Mann L, Krois J, Sälzer S, Kahl M, Springer C. Comparison of periodontitis patients’ classification in the 2018 versus 1999 classification. J Clin Periodontol. 2019;46(9):908-17. [Google Scholar]
- Murakami S, Mealey BL, Mariotti A, Chapple ILC. Dental plaque-induced gingival conditions. J Clin Periodontol. 2018;45(20):28-35. [Google Scholar]
- Abbott P. Classification, diagnosis and clinical manifestations of oral diseases. Endodontitis Topical. 2004;9(2):899-904. [Google Scholar]
- Dietrich T, Ower P, Tank M, West NX, Walter C, Needleman I. Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions – implementation in clinical practice. Br Dent J. 2019;226(1):16-22. [Google Scholar]
- Herrera D, Retamal-Valdes B, Alonso B, Feres M. Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J Periodontol. 2018;89(1):S85-S102. [Google Scholar]
- Gher M, Vermino AR. Root morphology- Clinical signifance in pathogenesis and treatment of dental plaque gingivitis. J Am Dent Assoc. 1990;12:36-41. [Google Scholar]
- Tonetti MS, Sanz M. Implementation of the new classification of periodontal diseases: Decision‐making algorithms for clinical practice and education. J Clin Periodontol. 2019;46(4):398-405. [Google Scholar]
- Rajeshwari HR, Dhamecha D, Jagwani S, Rao M, Jadhav K, Shaikh S. Local drug delivery systems in the management of periodontitis: A scientific review. J Controlled Release. 2019;307:393-409. [Google Scholar]
- Susin C, Haas AN, Albandar JM. Epidemiology and demographics of aggressive periodontitis. Periodontol. 2000;29(1):70-8. [Google Scholar]
- Petersen PE, Ogawa H. The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol. 2000;60(1):15-39. [Google Scholar]
- Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of Periodontitis in Adults in the United States: 2009 and 2010. J Dent Res. 2012;91(10):1449-54. [Google Scholar]
- Slots J, Neslon M. Systemic Diseases: facts, fallacies and the future. J Sci Res Dev. 2017;13(2):134-9. [Google Scholar]
- Dowsett SA, Archila L, Segreto VA, Eckert GJ, Kowolik MJ. Periodontal disease status of an indigenous population of Guatemala, Central America. J Clin Periodontol. 2001;72:1790-1800. [Google Scholar]
- Anusaksathien O, Sukboon A, Sitthiphong P, Teanpaisan R. Distribution of Interleukin-1β+3954and IL-1α–889Genetic Variations in a Thai Population Group. J Periodontol. 2003;74(12):1796-1802. [Google Scholar]
- Sundaram NS, Narendar R, Dineshkumar P, Ramesh SB, Gokulanathan S. Evaluation of oral health related quality of life in patient with mild periodontitis among young male population of Namakkal district. J Pharm Bioallied Sci. 2013;5(5):30-2. [Google Scholar]
- Rao S, Balaji SK, Lavu V. Chronic periodontitis prevalence and the inflammatory burden in a sample population from South India. Indian J Dent Res. 2018;29(2):254-9. [Google Scholar]
- Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontol. 2000;62(1):1049-52. [Google Scholar]
- Drago C. Treatment of Edentulous Patients with Immediate Occlusal Loading, Implant Restorations. . 2020;19:327-69. [Google Scholar]
- Taylor GW, Borgnakke WS. Periodontal disease: associations with diabetes, glycemic control and complications. Oral Diseases. 2008;14(3):191-6. [Google Scholar]
- Wadia R, Chapple I. Periodontal care in general practice: 20 important FAQs - Part two. BDJ Team. 2020;7(1):26-32. [Google Scholar]
- Kato T, Fujiwara N, Kuraji R, Numabe Y. Relationship between periodontal parameters and non-vital pulp in dental clinic patients: a cross-sectional study. BMC Oral Health. 2020;20(1):125-53. [Google Scholar]
- EKE PI, Borgnakke WS, Albandar JM. Measurement and Distribution of Periodontal diseases . Burt and Eklund's Dentistry. Dental Practice, and the Community. 2020. [Google Scholar]
- Berglundh T, Donati M. Aspects of adaptive host response in periodontitis. J Clin Periodontol. 2005;32(s6):87-107. [Google Scholar]
- Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol. 2015;15(1):30-44. [Google Scholar]
- Jepsen S, Suvan J, Deschner J. The association of Periodontal diseases with metabolic syndrome and obesity. Periodontol. 2000;83(1):3-12. [Google Scholar]
- Ji S, Choi Y. Microbial and Host Factors That Affect Bacterial Invasion of the Gingiva. J Dent Res. 2020;12:19-62. [Google Scholar]
- Costalonga M, Herzberg MC. The oral microbiome and the immunobiology of periodontal disease and caries. Immunol Lett. 2014;162(2):22-38. [Google Scholar]
- Meyle J, Dommisch H, Groeger S, Giacaman RA, Costalonga M, Herzberg M. The innate host response in caries and periodontitis. J Clin Periodontol. 2017;44(12):1215-25. [Google Scholar]
- Gu Y, Han X. Toll-Like Receptor Signalling and Immune Regulatory Lymphocyte in Periodontal Disease. Int J Mol Sci. 2020;21(9):3329-34. [Google Scholar]
- Chapple ILC, Weijden FVd, Doerfer C, Herrera D, Shapira L, Polak D. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol. 2015;42(16):S71-5. [Google Scholar]
- Carra MC, Gueguen A, Thomas F, Pannier B, Caligiuri G, Steg PG. Self-report assessment of severe periodontitis: Periodontal screening score development. J Clin Periodontol. 2018;45(7):818-31. [Google Scholar]
- Cole E, R–Chaudhuri A, Vaidyanathan M, Johnson J, Sood S. Simplified basic periodontal examination (BPE) in children and adolescents: a guide for general dental practitioners. Dent Update. 2014;41(4):328-7. [Google Scholar]
- Palmer RM, Floyd PD. Periodontology: A clinical approach: Periodontal examination and screening among different groups of Patients. Br Dent J. 1995;178(7):263-8. [Google Scholar]
- Oh TJ, Eber R, Wang HL. Periodontal diseases in the child and adolescent. J Clin Periodontol. 2002;29(5):400-10. [Google Scholar]
- Johnson TM, Worthington HV, Clarkson JE, Pericic TP, Sambunjak D, Imai P. Mechanical interdental cleaning for preventing and controlling periodontal diseases and dental caries (Protocol). Cochrane Database Syst Rev. 2015;12:21-9. [Google Scholar]
- Fine DH, Patil AG, Loos BG. Classification and diagnosis of aggressive periodontitis. J Clin Periodontol. 2018;45(20):S95-S111. [Google Scholar]
- Laine ML, Crielaard W, Loos BG. Genetic susceptibility to periodontitis. Periodontol. 2000;58(1):37-68. [Google Scholar]
- Nibali L, D’Aiuto F, Donos N, Griffiths GS, Parkar M, Tonetti MS. Association between periodontitis and common variants in the promoter of the interleukin-6 gene. Cytokine. 2009;45(1):50-4. [Google Scholar]
- Hine MK. The use of the toothbrush in the treatment of periodontitis. J Am Dent Assoc. 1950;41(2):158-68. [Google Scholar]
- Erbe C, Klees V, Braunbeck F, Ferrari-Peron P, Ccahuana-Vasquez RA, Timm H. Comparative assessment of plaque removal and motivation between a manual toothbrush and an interactive power toothbrush in adolescents with fixed orthodontic appliances: A single-center, examiner-blind randomized controlled trial. Am J Orthod Dentofac Orthop. 2019;155(4):462-72. [Google Scholar]
- Efstratiou M, Papaioannou W, Nakou M, Ktenas E, Vrotsos IA, Panis V. Contamination of a toothbrush with antibacterial properties by oral microorganisms. J Dent. 2007;35(4):331-7. [Google Scholar]
- Sanz I, Alonso B, Carasol M, Herrera D, Sanz M. . J Evid Based Dent Pract. 2012;47(3):18-26. [Google Scholar]
- Cleland WP. Nonsurgical periodontal therapy. Clin Tech Small Anim Pract. 2000;15(4):221-5. [Google Scholar]
- Friedman S, Abitbol S, Lawrence H. Treatment Outcome in Endodontics: The Toronto Study. Phase 1: Initial Treatment. J Endod. 2003;29(12):787-93. [Google Scholar]
- Jain N, Jain GK, Javed S, Iqbal Z, Talegaonkar S, Ahmad FJ. Recent approaches for the treatment of periodontitis. Drug Discovery Today. 2008;13(21-22):932-43. [Google Scholar]
- Cobb CM. Lasers and the treatment of periodontitis: the essence and the noise. Periodontology. 2000;75(1):205-295. [Google Scholar]
- Nowzari H. Aesthetic osseous surgery in the treatment of periodontitis. Periodontol 2000. 2001;27(1):8-28. [Google Scholar]
- Rohlin M, Susanna A, Ekman A, Klinge B, Larsson G. Chronic Periodontitis -Prevention, Diagnos and Treatment - A systematic review. SBU Syst Rev Summ. 2004;31:239-52. [Google Scholar]
- Durham J, Fraser HM, McCracken GI, Stone KM, John MT, Preshaw PM. Impact of periodontitis on oral health-related quality of life. J Dent. 2013;41(4):370-6. [Google Scholar]
- Dyke TEV. The Management of Inflammation in Periodontal Disease. J Periodontol. 2008;79(8s):1601-8. [Google Scholar]
- Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: The Toronto study. Phases I and II: Orthograde retreatment. J Endod. 2004;32:493-503. [Google Scholar]
- Siqueira JF, Rôças IN, Ricucci D, Hülsmann M. Causes and management of post-treatment apical periodontitis. Br Dent J. 2014;216(6):305-12. [Google Scholar]
- Abstract
- Background
- Stages
- Types of Periodontitis[15], [16], [17], [18]
- Gingivitis
- Chronic periodontitis
- Aggressive periodontitis
- Necrotizing ulcerative gingivitis
- Systemic chronic periodontitis
- Occurance & Epidemiology
- Pathophysiology
- Periodontal Screening and Examination[40], [41]
- General description like
- Periodontal screening using basic periodontal examination and recordings
- Detailed examination of ligament degradation and periodontal pocket depth as:
- Diagnosis[45], [46], [47]
- Treatment and Management
- Initial therapy
- Non-surgical treatment:[53], [54]
- Corrective therapy or surgical treatments[55], [56], [57], [58]
- Supportive therapy
- Clinical Significance
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Dubey P, Mittal N. Periodontal diseases- A brief review [Internet]. Int J Oral Health Dent. 2020 [cited 2025 Oct 28];6(3):177-187. Available from: https://doi.org/10.18231/j.ijohd.2020.038
APA
Dubey, P., Mittal, N. (2020). Periodontal diseases- A brief review. Int J Oral Health Dent, 6(3), 177-187. https://doi.org/10.18231/j.ijohd.2020.038
MLA
Dubey, Pragati, Mittal, Neelam. "Periodontal diseases- A brief review." Int J Oral Health Dent, vol. 6, no. 3, 2020, pp. 177-187. https://doi.org/10.18231/j.ijohd.2020.038
Chicago
Dubey, P., Mittal, N.. "Periodontal diseases- A brief review." Int J Oral Health Dent 6, no. 3 (2020): 177-187. https://doi.org/10.18231/j.ijohd.2020.038
